Ebola
| Ebola virus | |
|---|---|

| |
| Virus classification | |
| Group: | Group V ((−)ssRNA)
|
| Order: | |
| Family: | |
| Genus: | |
| Species: | |
| Ebola | |
|---|---|
| Specialty | Infectious diseases |
'Ebola' is both the common term used to describe a group of viruses belonging to genus Ebolavirus, family Filoviridae, and the common name for the disease which they cause, Ebola hemorrhagic fever. The viruses are characterised by a long, filamentous morphology and surrounded by a lipid viral envelope. Ebolaviruses are morphologically similar to the Marburg virus, also in the family Filoviridae, and share similar disease symptoms. It has caused a number of serious and highly publicized outbreaks since its discovery, as well as featuring as the gruesome antagonist in many forms of entertainment.
Ebola is believed to be a zoonotic virus. Despite considerable effort by the World Health Organization no animal reservoir capable of sustaining the virus between outbreaks has been identified. However, it has been hypothesized that the most likely candidate is the fruit bat.
In the absence of knowing where the reservoir lies, the World Health Organization has taken serious steps to ensure that all known Biosafety Level 4 agents (including Ebola) are carefully and properly contained.
Ebola hemorrhagic fever is potentially lethal and encompasses a range of symptoms including vomiting, diarrhea, general body pain, internal and external bleeding, and fever. Mortality rates are generally high, ranging from 50% - 90%, with the cause of death usually due to hypovolemic shock or organ failure.
Because Ebola is potentially lethal and since no approved vaccine or treatment is available, Ebola is classified as a biosafety level 4 agent, as well as a Category A bioterrorism agent by the Centers for Disease Control and Prevention. It has the potential to be weaponized for use during biological warfare and was investigated for this particular use by both the Soviet Union and the United States during the Cold War. Its efficacy as a biological-warfare agent is compromised by its extreme lethality and its quickness: a typical outbreak spreads through a small village or hospital, kills everyone there, and runs out of potential hosts, burning out before it reaches a larger community.
Etymology
The virus is named after the Ebola River Valley in the African nation-state of the Democratic Republic of the Congo (formerly Zaïre), near the site of the first recognized outbreaks in 1976.[1]
Structure

Size and shape
Electron micrographs of members of Ebolavirus show them to have the characteristic thread-like structure of a filovirus.[2] EBOV VP30 is around 288 amino acids long.[2] The virions are tubular and variable in shape and may appear as a "U", "6", coiled, circular, or branched shape, however, laboratory purification techniques, such as centrifugation, may contribute to the various shapes seen.[2] Virions are generally 80 nm in diameter.[2] They are variable in length, and can be up to 1400 nm long. On average, however, the length of a typical Ebola virus is closer to 1000 nm. In the center of the virion is a structure called nucleocapsid, which is formed by the helically wound viral genomic RNA complexed with the proteins NP, VP35, VP30 and L. It has a diameter of 40 – 50 nm and contains a central channel of 20–30 nm in diameter. Virally encoded glycoprotein (GP) spikes 10 nm long and 10 nm apart are present on the outer viral envelope of the virion, which is derived from the host cell membrane. Between envelope and nucleocapsid, in the so-called matrix space, the viral proteins VP40 and VP24 are located.
Genome
Each virion contains one minor molecule of linear, single-stranded, negative-sense RNA, totaling 18959 to 18961 nucleotides in length. The 3′ terminus is not polyadenylated and the 5′ end is not capped. It was found that 472 nucleotides from the 3' end and 731 nucleotides from the 5' end were sufficient for replication.[2] It codes for seven structural proteins and one non-structural protein. The gene order is 3′ - leader - NP - VP35 - VP40 - GP/sGP - VP30 - VP24 - L - trailer - 5′; with the leader and trailer being non-transcribed regions which carry important signals to control transcription, replication and packaging of the viral genomes into new virions. The genomic material by itself is not infectious, because viral proteins, among them the RNA-dependent RNA polymerase, are necessary to transcribe the viral genome into mRNAs, as well as for replication of the viral genome.
Replication
The viral attachment protein recognizes specific receptors, which may be protein, carbohydrate or lipid, on the outside of the cell. The mechanism of virus entry into host cells is unknown, but it is reasonable to assume that the glycoprotein spikes on the surface of the virion would mediate the process, as they are the only transmembrane protein present on the surface. The two types of GP, the other being sGP, are specific for different cell types.
The virus next activates and releases its own genetic material, causing the host to begin manufacturing the proteins necessary for virus reproduction using its own resources. This replication continues until the cell ruptures and bursts. The virus is then spread to neighboring cells, and continues this chain of reproduction until masses of host cells are damaged. The host then may die soon after. The spread of the virus through the population can be halted if the proper sterilization and quarantine measures are taken, as the only method by which the virus may continue to propagate is via direct contact with body fluids. In order for a successful infection the virus must first evade the immune system. One of the ways it does this is by inhibiting interferon activity. VP24 blocks IFN-α/β and IFN-γ signaling by interacting with karyopherin α1, the nuclear localization signal receptor for tyrosine-phosphorylated STAT1, preventing the formation of an interferon induced antiviral state. Another protein, VP35, blocks the transcription factor interferon regulatory factor 3 (IRF-3), which is important for the expression of IFN-α/β.
Ebola and Marburg viruses have RNA single base substitution rates approximately a hundred times slower than retroviruses and human influenza A virus. This significant difference is due to their replication with their own RNA-dependent RNA polymerases, as compared with rapidly mutating RNA viruses that use the error prone reverse transcriptase in their replication, such as HIV. This means ebola is, and will remain, genetically stable.[3] Chances of enough base mutations leading to formation of a new protein allowing airborne transmission are insignificant.
Species
Zaïre ebolavirus

The Zaïre Ebolavirus has the highest mortality rate, up to 90% in some epidemics, with an average of approximately 83% mortality over 27 years. The case-fatality rates were 88% in 1976, 100% in 1977, 59% in 1994, 81% in 1995, 73% in 1996, 80% in 2001-2002 and 90% in 2003. There have been more outbreaks of Zaïre Ebolavirus than any other strain.
The first outbreak took place on August 26, 1976 in Yambuku, a town in the north of Zaïre. The first recorded case was Mabalo Lokela, a 44-year-old schoolteacher returning from a trip around the north of the state. His high fever was diagnosed as possible malaria and he was subsequently given a quinine shot. Lokela returned to the hospital every day. A week later, his symptoms included uncontrolled vomiting, bloody diarrhea, headache, dizziness, and trouble breathing. Later, he began bleeding from his nose, mouth, and anus. Lokela died on September 8, 1976, roughly 14 days after the onset of symptoms.
Soon after, more patients arrived with varying but similar symptoms including fever, headache, muscle and joint aches, fatigue, nausea, and dizziness. These often progressed to bloody diarrhea, severe vomiting, and bleeding from the nose, mouth, and anus. The initial transmission was believed to be due to reuse of the needle for Lokela’s injection without sterilization. Subsequent transmission was also due to care of the sick patients without barrier nursing and the traditional burial preparation method, which involved washing and gastrointestinal tract cleansing.
Two Belgian nuns working in Yambuku as nurses also died in the same outbreak [4].
Sudan ebolavirus

Sudan Ebolavirus was the second strand of Ebola reported in 1976. It apparently originated amongst cotton factory workers in Nzara, Sudan. The first case reported was a worker exposed to a potential natural reservoir at the cotton factory. Scientists tested all animals and insects in response to this, however none tested positive for the virus. The carrier is still unknown.
A second case involved a nightclub owner in Nzara, Sudan. The local hospital, Maridi, tested and attempted to treat the patient; however, nothing was successful, and he died. The nurses did not apply safe and practical procedures in sterilizing and disinfecting the medical tools used on the nightclub owner, facilitating the spread of the virus in the hospital.
The most recent outbreak of Sudan Ebolavirus occurred in May 2004. As of May 2004, 20 cases of Sudan Ebolavirus were reported in Yambio County, Sudan, with 5 deaths resulting. The Centers for Disease Control and Prevention confirmed the virus a few days later. The neighbouring countries of Uganda and the Democratic Republic of Congo have increased surveillance in bordering areas, and other similar measures have been taken to control the outbreak. The average fatality rates for Sudan Ebolavirus were 53% in 1976, 68% in 1979, and 53% in 2000/2001. The average case-fatality rate is 53.76%.
Reston ebolavirus
First discovered in November of 1989 in a group of 100 Crab-eating macaques (Macaca fascicularis) imported from the Philippines to Reston, Virginia. A parallel infected shipment was also sent to Philadelphia. This strain was highly lethal in monkeys, but did not cause any fatalities in humans. Six of the Reston primate handlers tested positive for the virus, two due to previous exposure.
Further Reston Ebolavirus infected monkeys were shipped again to Reston, and Alice, Texas in February of 1990. More Reston Ebolavirus infected monkeys were discovered in 1992 in Siena, Italy and in Texas again in March 1996. A high rate of co-infection with Simian Hemorrhagic Fever (SHF) was present in all infected monkeys. No human illness has resulted from these two outbreaks.
Tai ebolavirus
This species of Ebola was first discovered amongst chimpanzees of the Tai Forest in Côte d’Ivoire, Africa. On November 1, 1994, the corpses of two chimpanzees were found in the forest. Necropsies showed blood within the heart to be liquid and brown, no obvious marks seen on the organs, and one presented lungs filled with liquid blood. Studies of tissues taken from the chimps showed results similar to human cases during the 1976 Ebola outbreaks in Zaïre and Sudan. Later in 1994, more dead chimpanzees were discovered, with many testing positive to Ebola using molecular techniques. The source of contamination was believed to be the meat of infected Western Red Colobus monkeys, which the chimpanzees preyed upon.[5]
One of the scientists performing the necropsies on the infected chimpanzees contracted Ebola. She developed symptoms similar to dengue fever approximately a week after the necropsy and was transported to Switzerland for treatment. After two weeks she was discharged from hospital, and was fully recovered six weeks after the infection.
Ebola hemorrhagic fever
Symptoms
Symptoms are varied and often appear suddenly. Initial symptoms include high fever (at least 38.8°C (~102°F)), severe headache, muscle, joint, or abdominal pain, severe weakness and exhaustion, sore throat, nausea, and dizziness[6]. Before an outbreak is suspected, these early symptoms are easily mistaken for malaria, typhoid fever, dysentery, influenza, or various bacterial infections, which are all far more common and less reliably fatal.
Ebola may progress to cause more serious symptoms, such as diarrhea, dark or bloody feces, vomiting blood, red eyes due to distention and hemorrhage of sclerotic arterioles, petechia, maculopapular rash, and purpura. Internal and external hemorrhage from orifices, such as the nose and mouth, may also occur, as well as from incompletely healed injuries such as needle-puncture sites. Hemorrhage is due to the virus having the ability to stop platelets from clotting and making the cell membranes permeable[citation needed]. Other secondary symptoms include hypotension (less than 90 mm Hg systolic /60 mm Hg diastolic), hypovolemia, tachycardia, organ damage (especially the kidneys, spleen, and liver) as a result of disseminated systemic necrosis, and proteinuria.
The span of time from onset of symptoms to death is usually between 7 and 14 days. By the second week of infection, patients will either defervesce (the fever will lessen) or undergo systemic multi-organ failure. Mortality rates are generally high, ranging from 50% - 90%[7]. The cause of death is usually due to hypovolemic shock or organ failure[8].
Filoviruses replicate well in a wide range of organs and cell types such as hepatocytes, epithelial cells, fibroblasts, fibroblastic reticular cells and adrenal cortical cells.[2] Most notably, the susceptibility of human endothelial cells is likely the cause of the symptoms that appear in the late stages of the infection such as shock syndrome and hemorrhaging.[2]
Transmission
Among humans, the virus is transmitted by direct contact with infected body fluids, or to a lesser extent, skin or mucus membrane contact. The incubation period can be anywhere from 2 to 21 days, but is generally between 5 and 10 days.
Although airborne transmission between monkeys has been demonstrated by an accidental outbreak in a laboratory located in Virginia, U.S.A, there is very limited evidence for human-to-human airborne transmission in any reported epidemics. Nurse Mayinga might represent the only possible case. The means by which she contracted the virus remain uncertain.
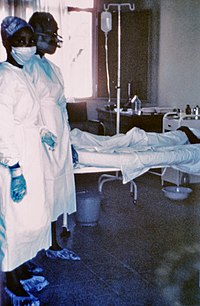
So far all epidemics of Ebola have occurred in sub-optimal hospital conditions, where practices of basic hygiene and sanitation are often either luxuries or unknown to caretakers and where disposable needles and autoclaves are unavailable or too expensive. In modern hospitals with disposable needles and knowledge of basic hygiene and barrier nursing techniques, Ebola rarely spreads on such a large scale.
In the early stages, Ebola may not be highly contagious. Contact with someone in early stages may not even transmit the disease. As the illness progresses, bodily fluids from diarrhea, vomiting, and bleeding represent an extreme biohazard. Due to lack of proper equipment and hygienic practices, large scale epidemics occur mostly in poor, isolated areas without modern hospitals or well-educated medical staff. Many areas where the infectious reservoir exists have just these characteristics. In such environments, all that can be done is to immediately cease all needle-sharing or use without adequate sterilization procedures, to isolate patients, and to observe strict barrier nursing procedures with the use of a medical rated disposable face mask, gloves, goggles, and a gown at all times. This should be strictly enforced for all medical personnel and visitors.
Ebola is limited on a global scale due to its difficulty in spreading by airborne transmission and the period of time that the virus can use a living and contagious victim to spread compared to other infectious diseases. In isolated settings such as a quarantined hospital or a remote village, most victims are infected shortly after the first case of infection is present. In addition, the quick onset of symptoms from the time the disease becomes contagious in an individual makes it easy to identify sick individuals and limits an individual's ability to spread the disease by traveling. Although bodies of the deceased are still infectious, many doctors implemented measures to properly dispose of dead bodies in spite of some traditional local burial rituals.[9]
Treatments

Treatment is primarily supportive and includes minimizing invasive procedures, balancing electrolytes, replacing lost coagulation factors to help stop bleeding, maintaining oxygen and blood levels, and treating any complicating infections. Despite some initial anecdotal evidence, blood serum from Ebola survivors has been shown to be ineffective in treating the virus. Interferon is also thought to be ineffective. Ribavirin is ineffective. In monkeys, administration of an inhibitor of coagulation (rNAPc2) has shown some benefit, protecting 33% of infected animals from a usually 100% (for monkeys) lethal infection. In early 2006, scientists at USAMRIID announced a 75% recovery rate after infecting four rhesus monkeys with Ebola virus and administering antisense drugs.[10]
Vaccines
Vaccines have been produced for both Ebola [11] and Marburg [12] that were 100% effective in protecting a group of monkeys from the disease. These vaccines are based on either a recombinant Vesicular stomatitis virus or a recombinant Adenovirus[13] carrying the Ebola spikeprotein on its surface. Early human vaccine efforts, like the one at NIAID in 2003, have so far not reported any successes.[14]
Viral reservoirs
Despite numerous studies, the wildlife reservoir of Ebolavirus has not been identified. Between 1976 and 1998, from 30,000 mammals, birds, reptiles, amphibians and arthropods sampled from outbreak regions, no Ebolavirus was detected[15] apart from some genetic material found in six rodents (Mus setulosus and Praomys species) and a shrew (Sylvisorex ollula) collected from the Central African Republic in 1998.[16] Ebolavirus was detected in the carcasses of gorillas, chimpanzees and duikers during outbreaks in 2001 and 2003 (the carcasses were the source of the initial human infections) but the high mortality from infection in these species precludes them from acting as reservoirs.[15]
Plants, arthropods and birds have also been considered as reservoirs, however bats are considered the most likely candidate[17]. Bats were known to reside in the cotton factory in which the index cases for the 1976 and 1979 outbreaks were employed and have also been implicated in Marburg infections in 1975 and 1980.[15] Of 24 plant species and 19 vertebrate species experimentally inoculated with Ebolavirus, only bats became infected.[18] The absence of clinical signs in these bats is characteristic of a reservoir species. In 2002-03, a survey of 1,030 animals from Gabon and the Republic of the Congo including 679 bats found Ebolavirus RNA in 13 fruit bats (Hyspignathus monstrosus, Epomops franquetti and Myonycteris torquata).[19] Bats are also known to be the reservoirs for a number of related viruses including Nipah virus, Hendra virus and lyssaviruses.
Weaponization
Because Ebola is lethal and since no approved vaccine or treatment is available, Ebola is classified as a Biosafety Level 4 agent, as well as a Category A bioterrorism agent[20] and a select agent by the CDC. Ebola was considered during biological warfare research at both Fort Detrick[21] in the United States and Biopreparat[22] in the Soviet Union during the Cold War.
Ebola shows potential as a biological weapon because of its lethality but due to its relatively short incubation period it may be more difficult to spread since it may kill its victim before it has a chance to be transmitted. As a result, some developers have considered breeding it with other agents such as smallpox[23] to create so-called chimera viruses.
As a terrorist weapon, Ebola has been considered by members of Japan's Aum Shinrikyo cult, whose leader, Shoko Asahara led about 40 members to Zaire in 1992 under the guise of offering medical aid to Ebola victims in what was presumably an attempt to acquire a sample of the virus.[24]
Cultural impact
This section needs expansion. You can help by making an edit requestadding to it . |
Ebola and Marburg have served as a rich source of ideas and plotlines for many forms of entertainment. The infatuation with the virus is likely due to the high mortality rate of its victims, its mysterious nature, and its tendency to cause gruesome bleeding from body orifices.
In the movie Outbreak the virus looks the same as the ebola virus.
Much of the representation of the Ebola virus in fiction and the media is considered exaggerated or myth.[citation needed] One pervasive myth follows that the virus kills so fast that it has little time to spread. Victims die very soon after contact with the virus. In reality, the incubation time is usually about a week. The average time from onset of early symptoms to death varies in the range 3-21 days, with a mean of 10.1. Although this would prevent the transmission of the virus to many people, it is still enough time for some people to catch the disease.
Another myth, portrayed by books like Germ by Robert Liparulo, states that the symptoms of the virus are horrifying beyond belief.[citation needed] In depictions of this type, victims of Ebola suffer from squirting blood, liquefying flesh, zombie-like faces and dramatic projectile bloody vomiting, at times, from even recently deceased. In actual fact, only a fraction of Ebola victims have severe bleeding that would be even somewhat dramatic to witness. The virus, although an engineered variant, is a major plot device, and is described much more accurately in the Tom Clancy novel Executive Orders. Approximately 10% of patients suffer some bleeding, but this is often internal or subtle, such as bleeding from the gums. Ebola symptoms are usually limited to extreme exhaustion, vomiting, diarrhea, abdominal pain, a high fever, headaches and other body pains.
The following is an excerpt from an interview with Philippe Calain, M.D. Chief Epidemiologist, CDC Special Pathogens Branch, Kikwit 1996:
At the end of the disease the patient does not look, from the outside, as horrible as you can read in some books. They are not melting. They are not full of blood. They're in shock, muscular shock. They are not unconscious, but you would say 'obtunded', dull, quiet, very tired. Very few were hemorrhaging. Hemorrhage is not the main symptom. Less than half of the patients had some kind of hemorrhage. But the ones that had bled, died.
See also
- Bolivian haemorrhagic fever
- Crimean Congo hemorrhagic fever (CCHF)
- Marburg haemorrhagic fever, the first known disease caused by a filovirus
- Matthew Lukwiya, Ugandan doctor at the forefront of the 2000 outbreak
References
- ^ Death Called a River Jason Socrates Bardi. Scribbs Research Institute. Retrieved 8 December 2006.
- ^ a b c d e f g Hans-Dieter K, Feldmann H. Ebola and Marburg Viruses, Molecular and Cellular Biology. 2004, Horizon Bioscience.
- ^ Suzuki, Y, Gojobori, T The origin and evolution of Ebola and Marburg viruses MOL BIOL EVOL 14 (8): 800-806 AUG 1997
- ^ http://www.itg.be/ebola/ebola-12.htm Two Belgian nurses died of Ebola
- ^ http://virus.stanford.edu/filo/eboci.html
- ^ WHO Fact Sheet Ebola haemorrhagic cold
- ^ WHO Fact Sheet Ebola haemorrhagic fever
- ^ Bray et al. “Ebola virus: the role of macrophages and dendritic cells in the pathogenesis of Ebola haemorrhagic fever.”, Int J Biochem Cell Biol. 2005 Aug, 37(8):1560-1566
- ^ "Dr. Matthew's Passion", New York Times, 18 February 2001
- ^ http://www.usamriid.army.mil/press%20releases/warfield_press_release.pdf
- ^ Jones et al. “Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses”, Nat Med. 2005 Jul, 11(7):786-790
- ^ Hevey et al. "Marburg virus vaccines based upon alphavirus replicons protect guinea pigs and nonhuman primates", Virology, 1998, 251:28-37
- ^ Sullivan et al. “Accelerated vaccination for Ebola virus haemorrhagic fever in non-human primates”, Nature 2003 Aug, 424(6949):602
- ^ NIAID Ebola Vaccine Enters Human Trial, November 18, 2003
- ^ a b c Pourrut, X, Kumulungui, B, Wittmann, T et al. (2005). The natural history of Ebola virus in Africa. Microbes and Infection. 7:1005–1014.
- ^ Morvan, JM, Deubel, V, Gounon, P et al. (1999). Identification of Ebola virus sequences present as RNA or DNA in organs of terrestrial small mammals of the Central African Republic. Microbes and Infection. 1:1193–1201.
- ^ Fruit bats may carry Ebola virus, BBC News, December 1, 2005
- ^ Swanepoel, R, Leman, PA, Burt, FJ. (1996). Experimental inoculation of plants and animals with Ebola virus. Emerging Infectious Diseases. 2:321–3215.
- ^ Leroy, EM, Kimulugui, B, Pourrut, X et al. (2005). Fruit bats as reservoirs of Ebola virus. Nature. 438:575–576.
- ^ Hoenen et al. “Ebola virus: unravelling pathogenesis to combat a deadly disease.”, Trends Mol. Med. 2006 May, 12(5):206-215
- ^ http://www.medicalnewstoday.com/medicalnews.php?newsid=6042,
- ^ http://www.technologyreview.com/read_article.aspx?ch=biotech&sc=&id=16485&pg=4
- ^ http://www.zkea.com/archives/archive02006.html
- ^ http://cns.miis.edu/pubs/reports/pdfs/aum_chrn.pdf
External links
Overviews
- Database entry on genus Ebolavirus - ICTVdB
- Ebola Virus Haemorrhagic Fever - Proceedings of an International Colloquium on Ebola Virus Infection and Other Haemorrhagic Fevers held in Antwerp, Belgium, 6-8 December, 1977
- Questions and Answers about Ebola Hemorrhagic Fever - Center for Disease Control (CDC), retrieved 10 July 2006
- WHO Factsheet - retrieved 10 July 2006
- Vaccine Research Center (VRC) - Information concerning Ebola vaccine research studies
Outbreaks
- Ebola 'kills over 5,000 gorillas' - BBC News, 8 December 2006. Retrieved 8 December 2006.
- History of Ebola Outbreaks - Centers for Disease Control Special Pathogens Branch, retrieved 10 July 2006
- Infection Control for Viral Hemorrhagic Fevers in the African Health Care Setting - Center for Disease Control and Prevention, Atlanta, December 1998
Infectivity
- Lethal experimental infection of rhesus monkeys with Ebola-Zaire (Mayinga) virus by the oral and conjunctival route of exposure PubMed, February 1996, Jaax et al.
- Lethal experimental infections of rhesus monkeys by aerosolized Ebola and marburg virus PubMed, August 1995
- Marburg and Ebola viruses as aerosol threats PubMed, 2004, USAMRIID
- Other viral bioweapons: Ebola and Marburg hemorrhag fever PubMed, 2004
- Transmission of Ebola virus (Zaire strain) to uninfected control monkeys in a biocontainment laboratory PubMed, December 1993
- What is the probability of a dangerous strain of Ebola mutating and becoming airborne? Brett Russel, retrieved 10 July 2006
