Human lung
It has been suggested that Borders of the lung be merged into this article. (Discuss) Proposed since August 2015. |
| Lung | |
|---|---|
 Detailed diagram of the lungs coloured for identification of the lobes | |
| Details | |
| System | Respiratory system |
| Identifiers | |
| Latin | pulmo |
| TA98 | A06.5.01.001 |
| TA2 | 3265 |
| FMA | 7195 |
| Anatomical terminology | |
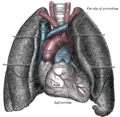
The lungs are the primary organs of respiration in humans and many other animals. Humans have two lungs, a right lung and a left lung. They are situated within the thoracic cavity of the chest. The right lung is bigger than the left lung, as the left lung shares space in the chest with the heart. The lungs together weigh approximately 1.3 kilograms (2.9 lb), with the right lung weighing more than the left. The lungs are part of the lower respiratory tract that begins at the trachea and branches into the bronchi and bronchioles and which receive air breathed in via the conducting zone. These divide until air reaches microscopic alveoli, which is where the process of gas exchange takes place. Together, the lungs contain approximately 2,400 kilometres (1,500 mi) of airways and 300 to 500 million alveoli.
The lungs are enclosed within a sac called the pleural sac which allows the inner and outer walls to slide over each other whilst breathing takes place, without much friction. This sac encloses each lung and also divides each lung into sections called lobes. The right lung has three lobes, whilst the left lung only has two. The lobes are further divided into bronchopulmonary segments and lobules. The tissues of the lungs have a unique blood supply, receiving deoxygenated blood sent from the heart for the purposes of receiving oxygen (the pulmonary circulation) and a separate blood supply of oxygenated blood (the bronchial circulation).
In fetal life, the lungs develop as an outpouching of the foregut, a tube which goes on to form the upper part of the digestive system. At this time, the fetus is situated in the amniotic sac and so the lungs do not function to breathe. Blood is also diverted from the lungs through the ductus arteriosus. At birth however, air begins to pass through the lungs, and the diversionary duct closes, so that the lungs can begin to respire. The lungs only fully develop in early childhood.
The tissue of the lungs can be affected by a number of diseases, including pneumonia and lung cancer. Chronic diseases such as chronic obstructive pulmonary disease and emphysema can be related to smoking or exposure to harmful substances. Diseases such as bronchitis can also affect the respiratory tract.
Structure
Gross anatomy
The lungs are located in the chest on either side of the heart in the rib cage. They stretch from close to the backbone in the rib cage, and rest on the diaphragm. The left lung shares space with the heart, with an angular notch in its anterior border called the cardiac notch. In addition, on the mediastinal surface of each lung there is a concavity called the cardiac impression at the level of the heart. The cardiac impression on the left lung is wider and deeper than that of the right lung. Because of this, and the cardiac notch, the right lung is larger in volume, total capacity and weight, despite being about 5cm shorter in height than the left. Both lungs have a central recession called the hilum at the root of the lung, where the blood vessels and airways pass into the lungs. There are also bronchopulmonary lymph nodes on the hilum. The costal surface along the rib cage is smooth and convex, with slight grooves corresponding to indentations by the ribs.
The lungs are surrounded by the pulmonary pleurae. The pleurae are two serous membranes; the outer parietal pleura lines the inner wall of the rib cage and the inner visceral pleura directly lines the surface of the lungs. Between the pleurae is a potential space called the pleural cavity containing pleural fluid. Each lung is divided into lobes by the invaginations of the pleura as fissures. The fissures are double folds of pleura that section the lungs. These sections help in the expansion of the lungs.[1]
The lobes of the lungs are further divided into bronchopulmonary segments based on the locations of bronchioles. Segments for the left and right lung are shown in the table.[2] The segmental anatomy is useful clinically for localizing disease processes in the lungs.[2]
Right lung
| Right lung | Left lung |
|---|---|
Upper
|
Upper
Lower
Lingula
|
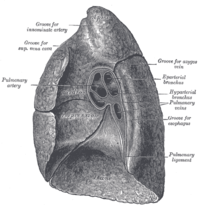
The right lung has both more lobes and segments than the left. It is divided into three lobes, an upper, middle, and a lower, by two fissures, one oblique and one horizontal. The upper, horizontal fissure, separates the upper from the middle lobe. It begins in the lower oblique fissure near the posterior border of the lung, and, running horizontally forward, cuts the anterior border on a level with the sternal end of the fourth costal cartilage; on the mediastinal surface it may be traced backward to the hilum.
The lower, oblique fissure, separates the lower from the middle and upper lobes, and is closely aligned with the oblique fissure in the left lung.[3] Its direction is, however, more vertical, and it cuts the lower border about 7.5 cm. behind its anterior extremity.
It has a deep concavity on its inner surface called the cardiac impression at the level of the heart. This is not as pronounced as that on the left lung where the heart projects further.
On this inner surface, above the hilum, is an arched groove at the level of the azygos vein; while running superiorly, and then arching laterally some little distance below the apex, is a wide groove for the superior vena cava and right innominate vein; behind this, and proximal to the apex, is a groove for the innominate artery. Behind the hilum and the attachment of the pulmonary ligament is a vertical groove for the esophagus. This groove becomes less distinct below, owing to the inclination of the lower part of the esophagus to the left of midline.
In front and to the right of the lower part of the esophageal groove is a deep concavity for the extrapericardiac portion of the thoracic part of the inferior vena cava.
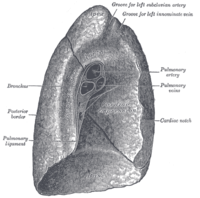
Left lung
The left lung is divided into two lobes, an upper and a lower, by the oblique fissure, which extends from the costal to the mediastinal surface of the lung both above and below the hilum. The left lung, unlike the right, does not have middle lobe, though it does have a homologous feature, a projection of the upper lobe termed the “lingula”. Its name means “little tongue”. The lingula on the left serves as an anatomic parallel to the right middle lobe, with both areas being predisposed to similar infections and anatomic complications.[4][5] There are two bronchopulmonary segments of the lingula: superior and inferior. It is thought that the lingula of the left lung is the remnant of the middle lobe, which has been lost in the course of evolution.
As seen on the surface, this fissure begins on the mediastinal surface of the lung at the upper and posterior part of the hilum, and runs backward and upward to the posterior border, which it crosses at a point about 6 cm. below the apex. It then extends downward and forward over the costal surface, and reaches the lower border a little behind its anterior extremity, and its further course can be followed upward and backward across the mediastinal surface as far as the lower part of the hilum. It has an angular indentation on the inner surface of its anterior border called the cardiac notch, and a concavity called the cardiac impression at the level of the heart. This is deeper and larger than that on the right, at which level the heart projects to the left.
On the same surface, immediately above the hilum, is a well-marked curved groove produced by the aortic arch. Running upward from this, toward the apex, is a groove at the level of the left subclavian artery. A slight impression in front of the latter, and close to the margin of the lung, lodges the left innominate vein. Behind the hilum and pulmonary ligament is a vertical groove produced by the descending aorta; in front of this, near the base of the lung, there is a shallow impression at the level of the lower esophagus.
Respiratory system

The lung is part of the respiratory system, and contains the majority of the lower respiratory tract after the trachea. The trachea receives air from the pharynx and travels down to a place where it splits (the carina) into a right and left bronchus. These supply air to the right and left lungs, splitting progressively into the secondary and tertiary bronchi for the lobes of the lungs, and into smaller and smaller bronchioles until they become the respiratory bronchioles. These in turn supply air through alveolar ducts into the alveoli, where the exchange of gasses take place. Oxygen diffuses through the walls of the alveoli into the capillaries (small blood vessels) nearby.
Estimates of the total surface area of lungs vary from 30-50 square metres[6] to up to 70-100 square metres (1076.39 sq ft) (8,4 x 8,4 m) in adults — which might be roughly the same area as one side of a tennis court.[7] However, such estimates may be of limited use unless qualified by a statement of scale at which they are taken (see coastline paradox and Menger sponge). Furthermore, if all of the capillaries that surround the alveoli were unwound and laid end to end, they would extend for about 992 kilometres (616 mi).
The parts of the respiratory system that conduct oxygen to the alveoli is called conducting zone, which is part of the respiratory tract, that conducts air into the lungs. This comprises the air passageways, with gas exchange only taking place in the alveoli of the respiratory system.
The bronchi in the conducting zone are reinforced with hyaline cartilage in order to hold open the airways. The bronchioles have no cartilage and are surrounded instead by smooth muscle. Air is warmed to 37 °C (99 °F), humidified and cleansed by the conduction zone; particles from the air being removed by the cilia which are located on the walls of all the passageways.
Blood supply
Being an organ of respiration, the human lung has a dual blood supply.
The tissue of the lungs receive oxygenated blood via the bronchial circulation, a series of arteries that leave the aorta and are part of the systemic circulation.
The lungs also receive deoxygenated blood from the heart and supply it with oxygen, in a process known as respiration. In this process, venous blood in the body collects in the right atrium and is pumped from the right ventricle through the pulmonary trunk and the pulmonary arteries into the left and right lungs. Blood passes through small capillaries next to the alveoli in the lung, receives oxygen, and travels back to the heart. This is called the pulmonary circulation. The oxygenated blood is then pumped to the rest of the body. Blood that leaves the heart is then returned to supply the tissues of the lung via the bronchial circulation mentioned above.
Microanatomy

Underneath the serous visceral pleura surrounding the lung is a subserous layer of areolar tissue and beneath this is the lung parenchyma.[8]Areolar tissue is a type of loose connective tissue characterised by a sparcity of fibroblasts with an abundance of interstitial fluid. This type of tissue acts as a reservoir of fluid, containing nutrients for the adjacent tissues which may be avascular. The parenchyma refers usually just to the alveolar tissue.
The lobule is the smallest microscopic unit of the lung. A lobule consists of a respiratory bronchiole, an alveolar duct, an alveolar sac, and alveoli.

Development

The development of the human lungs arise from the laryngotracheal groove and develop to maturity over several weeks inside the foetus and for several months following birth.[9] The larynx, trachea, bronchi and lungs begin to form during the fourth week of embryogenesis.[10] At this time, the lung bud appears ventrally to the caudal portion of the foregut. The location of the lung bud along the gut tube is directed by various signals from the surrounding mesenchyme, including fibroblast growth factors. At the same time as the lung bud grows, the future trachea separates from the foregut through the formation of tracheoesophageal ridges, which fuse to form the tracheoesophageal septum.
The lung bud divides into two, the right and left primary bronchial buds.[11] During the fifth week the right bud branches into three secondary bronchial buds and the left branches into two secondary bronchial buds. These give rise to the lobes of the lungs, three on the right and two on the left. Over the following week the secondary buds branch into tertiary buds, about ten on each side.[12] From the sixth week to the sixteenth week, the major elements of the lungs appear except the alveoli.[13] From week 16 to week 26, the bronchi enlarge and lung tissue becomes highly vascularised. Bronchioles and alveolar ducts also develop. During the period covering the 26th week until birth the important blood-air barrier is established. Specialised type I alveolar cells where gas exchange will take place, together with the type II alveolar cells that secrete pulmonary surfactant appear. The surfactant reduces the surface tension at the air-alveolar surface which allows expansion of the terminal saccules. These saccules form at the end of the bronchioles and their appearance marks the point at which limited respiration would be possible.[14]
First breath
At birth, the baby's lungs are filled with fluid secreted by the lungs and are not inflated. When the newborn is expelled from the birth canal, its central nervous system reacts to the sudden change in temperature and environment. This triggers it to take the first breath, within about 10 seconds after delivery.[15] The newborn lung is far from being a miniaturized version of the adult lung. It has only about 20,000,000 to 50,000,000 alveoli or 6 to 15 percent of the full adult compliment. Although it was previously thought that alveolar formation could continue to the age of eight years and beyond, it is now accepted that the bulk of alveolar formation is concluded much earlier, probably before the age of two years. The newly formed inter alveolar septa still contain a double capillary network instead of the single one of the adult lungs. This means that the pulmonary capillary bed must be completely reorganized during and after alveolar formation, it has to mature. Only after full microvascular maturation, which is terminated sometime between the ages of two and five years, is the lung development completed and the lung can enter a phase of normal growth.[16]
Function
Respiration

The respiratory system's alveoli are the sites of gas exchange with blood.
In humans, the trachea divides into the two main bronchi that enter the roots of the lungs. The bronchi continue to divide within the lung, and after multiple divisions, give rise to bronchioles. The bronchial tree continues branching until it reaches the level of terminal bronchioles, which lead to respiratory bronchioles and alveolar sacs. Alveolar sacs, are made up of clusters of alveoli, like individual grapes within a bunch. The individual alveoli are tightly wrapped in blood vessels and it is here that gas exchange actually occurs. Deoxygenated blood from the heart is pumped through the pulmonary artery to the lungs, where oxygen diffuses into blood and is exchanged for carbon dioxide in the hemoglobin of the erythrocytes. The oxygen-rich blood returns to the heart via the pulmonary veins to be pumped back into systemic circulation.[17]
- The sympathetic nervous system via noradrenaline acting on the beta receptors causes bronchodilation.
- The parasympathetic nervous system is through the vagus nerve,[18] via acetylcholine, which acts on the M-3 muscarinic receptors, maintains the resting tone of the bronchiolar smooth muscle. This action is related, although considered distinct from bronchoconstriction.
- Many other non-autonomic nervous and biochemical stimuli, including carbon dioxide and oxygen (acting on the respiratory centers), are also involved in the regulation process.
There is also a relationship noted between the pressures in the lung, in the alveoli, in the arteries and in the veins. This is conceptualised into the lung being divided into three vertical regions called the zones of the lung.[19]
Other
In addition to their function in respiration, the lungs also:
- Help in the regulation of blood pressure – as part of the renin-angiotensin system, the lungs convert angiotensin I to angiotensin II. In addition, they remove several blood-borne substances, such as a few types of prostaglandins, leukotrienes, serotonin and bradykinin.[20]
- Balance the pH of blood by facilitating alterations in the partial pressure of carbon dioxide
- Filter out small blood clots (and gas micro-bubbles formed during decompression) [21] from veins.
- Influence the concentration of some biologic substances and drugs used in medicine in blood
- May serve as a layer of soft, shock-absorbent protection for the heart, which the lungs flank and nearly enclose.
- Immunoglobulin-A is secreted in the bronchial secretion and protects against respiratory infections.
- Maintain sterility by producing mucus containing antimicrobial compounds.[22] Mucus contains glycoproteins, e.g., mucins, lactoferrin,[23] lysozyme, lactoperoxidase.[24][25] We find also on the epithelium Dual oxidase 2[26][27][28] proteins generating hydrogen peroxide, useful for hypothiocyanite endogenous antimicrobial synthesis. Function not in place in cystic fibrosis patient lungs.[29][30]
- Mucociliary clearance is an important defence system against air-borne infection. The dust particles and bacteria in the inhaled air are caught in the mucous layer present at the mucosal surface of respiratory passages and are moved up towards pharynx by the rhythmic upward beating action of the cilia.
- Provide airflow for the creation of vocal sounds.
- The lungs serve as a reservoir of blood in the body. The blood volume of the lungs is about 450 milliliters on average, about 9 percent of the total blood volume of the entire circulatory system. This quantity can easily fluctuate from between one-half and twice the normal volume. Loss of blood from the body due to hemorrhage can be partially compensated for by shunting blood from the lungs into the systemic circulatory vessels.[31]
Clinical significance
Human lungs can be affected by a variety of diseases. The environment of the lung is moist which makes it very hospitable to microorganisms. Many respiratory illnesses are due to infections from bacteria or viruses. Tuberculosis is a serious infection as is bacterial pneumonia. Pneumonia is an inflammatory condition of the lungs caused by infection. Pleurisy is an inflammatory condition of the pleurae surrounding the lungs usually caused by a viral infection from the lungs.

A pulmonary embolism is a blood clot that becomes lodged in the lung. A ventilation/perfusion scan using scintigraphy may be used to detect this.[32]
Lung diseases can arise suddenly, such as a pneumothorax or hemothorax, in which air or blood is trapped in the pleural cavity and compresses the lung. The accumulation of blood and other types of fluid in the pleural cavity can cause various types of pleural effusion which results in breathing difficulties.

Diseases can also be chronic, such as bronchitis and asthma, both of which are inflammatory diseases; and emphysema, a common complication of smoking caused by inflammation and the progressive inability of alveoli to expand and contract with respiration. Pulmonary fibrosis can occur when the lung is inflamed for a long period of time. This can be due to an occupational disease such as Coalworker's pneumoconiosis or more rarely to a reaction to medication. Fibrosis in the lung is the replacement of lung tissue by fibrous connective tissue which causes irreversible lung scarring and can prove fatal.
Asthma, chronic bronchitis, bronchiectasis and chronic obstructive pulmonary disease (COPD) are all obstructive lung diseases characterised by airway obstruction. Bitter taste receptors have been identified in lung tissue, which cause airways to relax when a bitter substance is encountered. This mechanism is believed to be evolutionary adaptive since it helps to clear lung infections and could be exploited to treat asthma and COPD.[33]
Lung cancer can often be incurable. Also cancers in other parts of the body can be spread via the bloodstream and end up in the lungs where the malignant cells can metastasise.
An azygos lobe is a congenital anatomical variation which though usually without effect can cause problems in thoracoscopic procedures.[34]
Lung volumes

Lungs have a tremendous reserve volume as compared to the oxygen exchange requirements when at rest. Such excess capacity is one of the reasons that individuals can smoke for years without having a noticeable decrease in lung function while still or moving slowly; in situations like these only a small portion of the lungs are actually perfused with blood for gas exchange. Destruction of too many alveoli over time leads to the condition emphysema, which is associated with extreme shortness of breath. As oxygen requirements increase due to exercise, a greater volume of the lungs is perfused, allowing the body to match its carbon dioxide-oxygen exchange requirements. Additionally, due to the excess capacity, it is possible for humans to live with only one lung, with the one compensating for the other's loss.
Lung volumes and lung capacities include inspiratory reserve volume, tidal volume, functional residual capacity, expiratory reserve volume, and residual volume.[35]Pulmonary plethysmographs are used to measure functional residual capacity. The total lung capacity depends on the person's age, height, weight, and sex, and normally ranges between 4,000 and 6,000 cm3 (4 to 6 L). Females tend to have a 20–25% lower capacity than males. Tall people tend to have a larger total lung capacity than shorter people. Smokers have a lower capacity than nonsmokers. Lung capacity is also affected by altitude. People who are born and live at sea level will have a smaller lung capacity than people who spend their lives at a high altitude. In addition to the total lung capacity, the tidal volume is also measured, this is the volume breathed in with an average breath, which is about 500 cm3.[36]
Another measure is the respiratory minute volume which is the volume of air which can be inhaled or exhaled from a person's lungs in one minute. This is normally registered when a person has a ventilator supporting breathing due to a sickness or injury. Other lung function tests include spirometry, measuring the amount (volume) and flow of air that can be inhaled and exhaled. The maximum volume of breath that can be exhaled is called the vital capacity. These tests can help to determine whether a disease is restrictive or obstructive.
See also
Additional images
-
Diagram of the respiratory system
-
Anatomy of lungs
-
Front view of heart and lungs
-
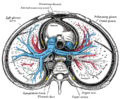
Transverse section of thorax, showing relations of pulmonary artery
-
Human embryo, 38 mm, 8–9 weeks.
References
![]() This article incorporates text in the public domain from page 1093 of the 20th edition of Gray's Anatomy (1918)
This article incorporates text in the public domain from page 1093 of the 20th edition of Gray's Anatomy (1918)
- ^ "Lung fissures". http://radiopaedia.org/articles/lung-fissures.
{{cite web}}: External link in|website=|url=(help) - ^ a b c Arakawa, H; Niimi, H; Kurihara, Y; Nakajima, Y; Webb, WR (December 2000). "Expiratory high-resolution CT: diagnostic value in diffuse lung diseases". AJR. American journal of roentgenology. 175 (6): 1537–43. PMID 11090370.
- ^ "Lung fissures". http://radiopaedia.org/articles/lung-fissures.
{{cite web}}: External link in|website=|url=(help) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 21324708, please use {{cite journal}} with
|pmid=21324708instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 14718418, please use {{cite journal}} with
|pmid=14718418instead. - ^ PS Haselton (May 16, 1972). "Journal of Anatomy". Journal of Anatomy. 112 (Pt 3). Journal of Anatomy: 391–400. PMC 1271180. PMID 4564685.
- ^ Notter, Robert H. (2000). Lung surfactants: basic science and clinical applications. New York, N.Y: Marcel Dekker. p. 120. ISBN 0-8247-0401-0. Retrieved 2008-10-11.
- ^ Dorland's (2012). Dorland's Illustrated Medical Dictionary (32nd ed.). Elsevier. p. 1077. ISBN 978-1-4160-6257-8.
- ^ Sadler T (2003). Langman's Medical Embryology (9th ed.). Lippincott Williams & Wilkins. ISBN 0-7817-4310-9.
- ^ Moore KL, Persaud TVN (2002). The Developing Human: Clinically Oriented Embryology (7th ed.). Saunders. ISBN 0-7216-9412-8.
- ^ Larsen WJ. Human Embryology 2001.Page 144
- ^ Larsen WJ. Human Embryology 2001. Page 144
- ^ Kyung Won, PhD. Chung (2005). Gross Anatomy (Board Review). Hagerstown, MD: Lippincott Williams & Wilkins. p. 156. ISBN 0-7817-5309-0.
- ^ Dorlands Medical Dictionary 2012 Page 1660
- ^ About.com > Changes in the newborn at birth Review Date: 27 November 2007. Reviewed By: Deirdre OReilly, MD
- ^ Burri, P (n.d). lungdevelopment. Retrieved March 21, 2012, from www.briticannica.com/EBchecked/topic/499530/human-respiration/66137/lung-development
- ^ "Lung Disease & Respiratory Health Center".
- ^ http://web.carteret.edu/keoughp/LFreshwater/PHARM/Blackboard/PNS/Neural%20Control%20of%20Lung%20Function.htm
- ^ Permutt S, Bromberger-Barnea B, Bane H.N (1962). "Alveolar Pressure, Pulmonary Venous Pressure, and the Vascular Waterfall". Med. Thorac. 19 (4): 239–269. doi:10.1159/000192224.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Walter F., PhD. Boron (2004). Medical Physiology: A Cellular And Molecular Approach. Elsevier/Saunders. ISBN 1-4160-2328-3. Page 605
- ^ Wienke B.R.: "Decompression theory"[verification needed]
- ^ Travis SM, Conway BA, Zabner J, et al. (May 1999). "Activity of abundant antimicrobials of the human airway". American Journal of Respiratory Cell and Molecular Biology. 20 (5): 872–9. doi:10.1165/ajrcmb.20.5.3572. PMID 10226057.
- ^ Rogan MP, Taggart CC, Greene CM, Murphy PG, O'Neill SJ, McElvaney NG (October 2004). "Loss of microbicidal activity and increased formation of biofilm due to decreased lactoferrin activity in patients with cystic fibrosis". The Journal of Infectious Diseases. 190 (7): 1245–53. doi:10.1086/423821. PMID 15346334.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Wijkstrom-Frei C, El-Chemaly S, Ali-Rachedi R, et al. (August 2003). "Lactoperoxidase and human airway host defense". American Journal of Respiratory Cell and Molecular Biology. 29 (2): 206–12. doi:10.1165/rcmb.2002-0152OC. PMID 12626341.
- ^ Conner GE, Salathe M, Forteza R (December 2002). "Lactoperoxidase and hydrogen peroxide metabolism in the airway". American Journal of Respiratory and Critical Care Medicine. 166 (12 Pt 2): S57–61. doi:10.1164/rccm.2206018. PMID 12471090.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Fischer H (October 2009). "Mechanisms and Function of DUOX in Epithelia of the Lung". Antioxidants & Redox Signaling. 11 (10): 2453–65. doi:10.1089/ARS.2009.2558. PMC 2823369. PMID 19358684.
- ^ Rada B, Leto TL (2008). "Oxidative innate immune defenses by Nox/Duox family NADPH Oxidases". Contributions to Microbiology. Contributions to Microbiology. 15: 164–87. doi:10.1159/000136357. ISBN 978-3-8055-8548-4. PMC 2776633. PMID 18511861.
- ^ Rada B, Lekstrom K, Damian S, Dupuy C, Leto TL (October 2008). "The Pseudomonas toxin pyocyanin inhibits the Dual oxidase-based antimicrobial system as it imposes oxidative stress on airway epithelial cells". Journal of Immunology. 181 (7): 4883–93. doi:10.4049/jimmunol.181.7.4883. PMC 2776642. PMID 18802092.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Moskwa P, Lorentzen D, Excoffon KJ, et al. (January 2007). "A Novel Host Defense System of Airways Is Defective in Cystic Fibrosis". American Journal of Respiratory and Critical Care Medicine. 175 (2): 174–83. doi:10.1164/rccm.200607-1029OC. PMC 2720149. PMID 17082494.
- ^ Conner GE, Wijkstrom-Frei C, Randell SH, Fernandez VE, Salathe M (January 2007). "The Lactoperoxidase System Links Anion Transport To Host Defense in Cystic Fibrosis". FEBS Letters. 581 (2): 271–8. doi:10.1016/j.febslet.2006.12.025. PMC 1851694. PMID 17204267.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ GUYTON&HALL Medical physiology 12th edition
- ^ Hofman, MS; Beauregard, JM; Barber, TW; Neels, OC; Eu, P; Hicks, RJ (October 2011). "68Ga PET/CT ventilation-perfusion imaging for pulmonary embolism: a pilot study with comparison to conventional scintigraphy". Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 52 (10): 1513–9. PMID 21908388.
- ^ Taste Receptors | University of Maryland Medical Center
- ^ [1]
- ^ Weinberger SE (2004). Principles of Pulmonary Medicine (4th ed.). Saunders. ISBN 0-7216-9548-5.
- ^ Maton, Anthea; Jean Hopkins; Charles William McLaughlin; Susan Johnson; Maryanna Quon Warner; David LaHart; Jill D. Wright (1993). Human Biology and Health. Englewood Cliffs, New Jersey, USA: Prentice Hall. ISBN 0-13-981176-1.