Saratani ya mapafu
| Lung cancer | |
|---|---|
| Mwainisho na taarifa za nje | |
| Kundi Maalumu | Oncology, pulmonology |
| ICD-10 | C33.-C34. |
| ICD-9 | 162 |
| DiseasesDB | 7616 |
| MedlinePlus | 007194 |
| eMedicine | med/1333 med/1336emerg/335radio/807radio/405radio/406 |
| MeSH | D002283 |
Saratani ya mapafu ni ugonjwa unaohusishwa na ukuaji wa seli katika tishu za mapafu. Tishu hii isipotibiwa, inaweza kuenea kwa njia inayoitwa metastasisi kwa tishu zilizokaribu au kwa mwili. Saratani zinazoanzia kwa mapafu, ziitwazo saratani za kwanza, ni kasinomasi zinazotoka kwa seli za epitheliumu. Aina kuu za saratani ni kasinoma ya mapafu ya seli ndogo (KMSN), pia huitwa saratani ya seli ya oat, na kasinoma ya mapafu ya seli kubwa (KMSK). Dalili inayojulikana sana ni kukohoa (pamoja na kukohoa damu), kupoteza uzito na upungufu wa pumzi.[1]
Kisababishi kikuu cha saratani ya mapafu ni kuathiriwa na moshi wa tumbaku,[2] unaosababisha asilimia 80–90 ya saratani.[1] Wasiovuta huchangia visa hivi kwa asilimia 10-15–[3] na mara nyingi huhusishwa na muungano wa masuala ya kijenetiki,[4] gesi ya radoni,[4] asbesto,[5] na uchafuzi wa hewa[4] pamoja na moshi kutoka kwa anayevuta sigara.[6][7] Saratani ya mapafu inaweza kuonekana kwa rediografu ya kifua na tomografi ya kompyuta (ukaguzi wa CT). utambuzi hudhibitishwa kwa biopsi[8] ambao hutekelezwa kwa bronkoskopi au mwongozo wa CT. Matibabu na matokeo ya muda mrefu hulingana na aina ya saratani, hatua (kiwango cha uenezi), na afya kwa jumla ya mtu, ikipimwa kwa hali ya utendakazi.
Matibabu ya kawaida ni pamoja na upasuaji, kemotherapi, na radiotherapi. KMSK wakati mwingine hutibiwa na upasuaji, ilhali KMSN huwa bora kwa kemotherapi na radiotherapi.[9] Kwa jumla, asilimia 15 ya waliopatikana na saratani nchini Marekani wana kuishi miaka mitano.[10] Ulimwenguni kote, saratani ya mapafu ni kisababishi cha kawaida cha vifo vinavyohusiana na saratani kwa wanaume na wanawake, na husababisha Vifo milioni 1.38 kwa mwaka, kufikia 2008.[11]
Ishara na dalili
[hariri | hariri chanzo]Ishara na dalili zinazoashiria saratani ya mapafu ni pamoja na:[1]
- Dalili za upumuaji: kukohoa, kukohoa damu, kukoroma au upungufu wa pumzi
- Dalili za kimfumo: kupoteza uzito, homa, kupindika kwa kucha za vidole, au uchovu
- Dalili kwa sababu ya kugandamizwa : maumivu ya kifua, maumivu ya mifupa, kuzibwa kwa vena kubwa, matatizo ya kumeza
Ikiwa saratani itatokea katika njia ya hewa, inaweza kuziba mpito wa hewa, na kusababisha matatizo ya kupumua. Uzibaji unaweza kusababisha mkusanyiko wa unyesaji nyuma ya kizibo, na kuwa nimonia.[1]
Kulingana na aina ya tyuma, inayoitwa fenomena ya paraneoplastiki inaweza kuleta magonjwa.[12] Katika saratani ya mapafu, nimonia zinaweza kuwa pamoja na Sindromu ya Lambert–Eaton myasthenic (udhaifu wa misuli kwa sababu ya autoantibodies), hipakalkemia, au sindromu ya homoni ya antidiuretic isiyofaa (SHAI). Tyuma katika ncha ya mapafu, inayoitwa tyuma ya Pancoast, inaweza kuingilia sehemu ya mfumo neva wa simpathetiki, na kusababisha sindromu ya Horner (kuanguka kwa kikawa cha jicho na mboni kwa upande huo), na kuharibika kwa brachial plexus.[1]
Dalili nyingi za saratani hii (kukosa hamu ya chakula, kupoteza uzito, homa, uchovu) si bayana.[8] Kwa wengi, saratani tayari imeenea zaidi kabla ya kuwa na dalili na kutafuta matibabu. Sehemu za kawaida inayoenea ni pamoja na ubongo, mifupa, adrenal gland, pafulililo mkabala, ini, perikadiumu, na figo.[13] Takribani asilimia 10 ya watu walio na saratani hawana dalili wakati wa utambuzi; saratani hizi hupatikana wakati wa radiotherapi ya kifua.[10]
Visababishi
[hariri | hariri chanzo]Saratani hujitokeza kufuatia kuharibika kwa jenetiki kwa DNA. Hii huathiri utendakazi wa seli, pamoja na seli inayozaa, kufa kwa seli (apoptosis) na urekebishaji wa DNA. Uharibikaji unapoongezeka, ndivyo hatari ya saratani inavyoongezeka .[14]
Uvutaji wa sigara
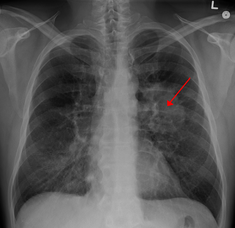
[hariri | hariri chanzo]Grafu inayoonyesha jinsi ongezeko la uuzaji wa tumbaku nchini Marekani katika miongo ya minne ya kwanza karne ya 20 (sigara anazovuta mtu mmoja kwa mwaka) ilisababisha ongezeko la haraka linalolingana na kiwango cha saratani ya mapafu wakati wa miaka ya 1930, 40, na 50 (vifo vya saratani kwa wanaume 100,000 kila mwaka [[File:saratani ya mapafu.jpg|kidole cha thumb|Picha ya pafu la binadamu: Eneo nyeupe katika ndewe ya juu ni saratani; Maeneo nyeusi ni kugeuka kwa rangi unaosababishwa na uvutaji. Uvutaji, haswa sigara, ni kisababishi kikuu cha saratani ya mapafu.[15] Moshi wa sigara huwa na kasinojeni zaidi ya 60 inayojulikana,[16] ikijumuisha radioisotopu kutoka uozaji wa radoni, nitrosamine, na benzopyrene. Kwa kuongeza, nikotini huonekana kuvunja matokeo ya kinga kwa uvimbe wa saratani kwa tishu zilizowazi.[17] Katika nchi zilizoendelea, asilimia 90 ya vifo vya saratani kwa wananume mwaka wa 2000 zilihusishwa na uvutaji wa sigara (asilimia 70 kwa wanawake).[18] Uvutaji huchangia kwa asilimia 80-90 ya visa vya saratani.[1]
Uvutaji wa moshi kutoka kwa anayevuta sigara—uvutaji moshi kutoka kwa mvuta siagara—ni kisababishi cha saratani kwa wasiovuta sigara. Mtu asiyevuta anaweza kuainishwa kama mtu anayeishi au kufanya kazi na mvutaji. Utafiti kutoka Marekani,[19][20] Ulaya,[21] Uingereza,[22] na Australia[23] Umeonyesha ongezeko kubwa la hatari kati ya wasiovuta sigara.[24] Wanaoishi na mvuta sigara huwa na asilimia 20–na 30 ya ongezeko la hatari ilhali wanaofanya kazi katika mazingira yalio na moshi uliovutwa wana asilimia 16–19 ya ongezeko la hatari.[25] Uchunguzi kuhusu moshi kutoka kwa wanaovuta unadokeza kuwa ni hatari zaidi kuliko moshi anaovuta mvutaji mwenyewe.[26] Uvutaji wa moshi husababisha takribani vifo 3,400 kutokana na saratani ya mapafu kila mwaka nchini marekani.[20]
Gesi ya Radoni
[hariri | hariri chanzo]Radoni ni gesi isiyo na rangi na harufu inayotokana na kuharibika kwa mnururisho radiumu, ambayo ni bidhaa zilizooza za urani, zinazopatikana katika umbo la ardhi. Bidhaa za mnururisho zilizooza ioni vitu vya jenetiki, vikisababisha mabadiliko yanayoleta saratani. Radoni ni kisababishi cha pili cha kawaida cha saratani nchini Marekani baada ya uvutaji wa sigara.[20] Hatari huongezeka asilimia 8–16 kwa kila ongezeko la 100 Bq/m³ katika kuwepo kwa radoni .[27] Viwango vya gesi ya radoni hutofautiana kulingana na maeneo na elementi za mchanga ulio chini na miamba. Kwa mfano, katika maeneo kama Cornwall nchini Uingereza (iliyo na granite kama safu ya chini), gesi ya radoni ni tatizo kuu, na majengo yanafaa kuwa na matundu ya kupitishia hewa na fani ili kupunguza kiwango cha gesi ya radoni. United States Environmental Protection Agency Hukadiria kuwa moja kwa maboma 15 nchini Marekani huwa na viwango vya radoni zaidi ya miongozo iliyopendekezwa ya picocurie 4 kwa kila lita (pCi/l) (148 Bq/m³).[28]
Asbesto
[hariri | hariri chanzo]Asbesto inaweza kusababisha baadhi ya magonjwa ya mapafu, pamoja na saratani yake. Uvutaji wa tumbaku na asbesto huwa na athari ya inayoshirikiana kuanza kwa saratani ya mapafu.[5] Pia inaweza kusababisha saratani ya pleura, inayoitwa mesothelioma (ambayo ni tofauti na saratani ya mapafu).[29]
Kuchafuka kwa hewa
[hariri | hariri chanzo]Kuchafuka kwa hewa huwa na athari ndogo kwa ongezeko la hatari ya saratani ya mapafu.[4] chembe (PM2.5) na sulfate aerosols, inayoweza kutoka kwa ekzozi ya magari barabarani, huhusishwa na hatari kidogo.[4][30] Kwa naitrojeni dioksidi, ongezeko la Sehemu 10 kwa kila bilioni huongeza hatari kwa asilimia 14.[31] Kuchafuka kwa hewa huchangia karibu asilimia 1-2 ya saratani.[4]
Pendekezo la dhibitisho kuunga mkono ongezeko la hatari ya saratani kutoka kwa uchafuzi wa hewa unaohusiana na kuchoma kuni, makaa, kinyesi cha mnyama, au mabaki yao ili kupika au kupasha joto.[32] Wanawake wanaoathiriwa na moshi ya makaa huwa na hatari mara dufu kama baadhi ya mabaki ya kuchoma biomasi yanajulikana au ni kasinojeni zinazodhaniwa.[33] Hatari hii huathiri takribani watu bilioni 2.4 ulimwenguni,[32] Na kuchangia asilimia 1.5 ya vifo vya saratani ya mapafu.[33]
Jenetikia
[hariri | hariri chanzo]Inakadiriwa kuwa asilimia 8 hadi 14 ya saratani ya mapafu husababishwa na masuala ya kuurithi.[34] Kwa jamaa walio na saratani, hatari huongezeka mara 2.4. Hii inawezekana kwa sababu ya mchanganyiko wa jeni.[35]s
Visababishi vingine
[hariri | hariri chanzo]Vitu vingine, Kazi, na maeneo mbalimbali yamehusishwa na saratani ya mapafu. International Agency for Research on Cancer (IARC) unaeleza kuwa "dhibitisho tosha" kuonyesha yafuatayo ni pafu lililo na kasinojeni:[36]
- Metali zingine (Utengenezaji wa aluminiamu, cadmium na elementi za kadimiamu, chromium(VI), beryllium na beriliamu, kupatikana kwa chuma na chuma cha pua, elementi za nikeli, arsenic na za aseniki isiyo hai, uchimbaji madini wa chini ya ardhi hematite)
- Bidhaa zingine za mwako (mwako usiokamilika, makaa ya moto (moshi wa ndani kutokana na kuchoma makaa kwa nyumba), kugeuza makaa kuwa gesi, kuweka lami, utengenezaji wa makaa, masizi, utoaji dizeli kutoka kwa injini
- Mnururisho aionishi (X-radiasheni, radoni-222 na vitu vyake vilivyooza, mnururisho wa gama, plutonium)
- Gesi sumu ingine (methyl ether (technical grade), Bis-(chloromethyl) ether, sulfurmustard, MOPP (vincristine-prednisone-nitrogen mustard-procarbazine mixture), harufu kali ya moshi kutokana na upakaji wa rangi)
- Utengenezaji wa raba na kristalini vumbi ya silika
Pathojenesisi
[hariri | hariri chanzo]Sawa na saratani nyingine nyingi, saratani ya mapafu huanzishwa na uhai wa oncogene au kutokuwa hai kwa jeni inayokandamiza tyuma.[37] Oncogenes zinaaminiwa huwafanya watu kuwa na uwezekano zaidi wa kupata saratani. Proto-oncogene zinaaminiwa kubadilika kuwa oncogenes zinapokutana na kasinojeni fulani.[38] Mabadiliko katika K-ras proto-oncogene husababisha asilimia 10–30 ya adenocarcinomas ya mapafu.[39][40] kipokezi cha suala la ukuaji wa epidemisi (KSUE) hudhibiti uzaaji wa seli, apoptosis, angiogenesis, na uvamizi wa tyuma.[39] Mabadiliko na ukuaji wa KSUE hupatikana sana katika saratani ya seli kubwa ya mapafu na hupeana msingi wa kutibu kwa vizuizi vya KSUE. Her2/neu huathirika mara chache.[39] Uharibifu wa Chromosomal unaweza kusababisha kukosekana kwa heterozygosity. Hii inaweza kusababisha kutotenda kazi kwa jeni zinazokandamiza tyuma. Kuharibika kwa chromosome 3p, 5q, 13q, na 17p ni kawaida hasa kwa kasinoma ya seli ndogo ya mapafu.p53 jeni inayokandamiza tyuma, iliyo kwa kromosomu 17p, huathirika katika asilimia 60-75 ya visa.[41] Jeni zingine ambazo mara nyingi hubadilika au kukua ni c-MET, NKX2-1, LKB1, PIK3CA, naBRAF.[39]
Utambuzi
[hariri | hariri chanzo][[Picha:Thorax CT peripheres Brronchialcarcinom li OF.jpg|kidole cha thumb|Ukaguzi wa CTkuonyesha tyuma ya saratani katika pafu la kushoto]] Kutekeleza radiotherapi ya kifua ni hatua ya kwanza ya uchunguzi ikiwa mtu ata ripoti dalili zinazoweza kuashiria saratani ya mapafu. Hii inaweza kuonyesha kupanuka kwa mediastinum (dokezo la kuenea kwa nodi ya limfu), atelectasis (kuvunjika), kuimarika (nimonia), au pleural effusion.[2] Upigaji picha wa CT hutumiwa kupeana habari zaidi kuhusu aina na kiwango cha maradhi. Bronkoskopi au mwongozo wa CT biopsi mara nyingi hutumiwa kuchukua sampuli ya tyuma ili kufanyia histopatholojia.[10]
Saratani ya mapafu hutokea kama nodu moja ya mapafu katika radiografu ya kifua. Hata hivyo, utambuzi wa kutofautisha ni mpana. Magonjwa mengine yanaweza kujitokeza hivi, pamoja na kifua kikuu, maambukizi ya kuvu, saratani ya metastasisi, au nimonia. Kisababishi kisicho cha kawaida cha nodu moja ya mapafu hujumuisha hamartoma, bronchogenic cyst, adenoma, ulemavu wa ateri na vena, pulmonary sequestration, rheumatoid nodule, Wegener's granulomatosis, au limfoma.[42] Saratani ya mapafu pia inaweza kuwa utambuzi wa dharura, kama kifundo kimoja cha mapafu katika radiografu ya kifua au ukaguzi wa CT uliotekelezwa kwa sababu isiyohusiana.[43] Utambuzi wa kufafanua saratani ya mapafu huzingatia histolojia uchunguzi wa tishu inayodhaniwa katika muktadha wa sifa za kliniki na radiolojia.[1]
Uainishaji
[hariri | hariri chanzo]| Histological type | Incidence per 100,000 per year |
|---|---|
| All types | 66.9 |
| Adenocarcinoma | 22.1 |
| Squamous-cell carcinoma | 14.4 |
| Small-cell carcinoma | 9.8 |
Saratani ya mapafu zimeainishwa kulingana na aina ya histolojia.[8] Uainishaji huu ni muhimu kwa kubainisha udhibiti na kubashiri matokeo ya maradhi. Saratani nyingi za mapafu ni ya kasinoma—hatari inayotokana na seli za epithelia. Kasinoma ya mapafu huainishwa kwa ukubwa na jinsi seli hatari zinavyoonekana ikiangaliwa na histopatholojia kwa darubini. Aina zote mbili ni kasinoma ya mapafu ya seli ndogo na kasinoma ya mapafu ya seli kubwa.[44]
Kasinoma ya mapafu ya seli kubwa
[hariri | hariri chanzo]
Aina tatu ndogo za KMSK ni adenocarcinoma, kasinoma ya mapafu ya seli za squamous, na kasinoma ya mapafu ya seli ndogo.[1]
Karibu asilimia 40 ya saratani huwa adenocarcinoma, ambayo kwa kawaida huanzia kwa tishu ya mapafu iliyo pembeni.[8] Visa vingi vya adenocarcinoma huhusishwa na uvutaji; hata hivyo, kati ya watu waliovuta sigara chini ya 100 katika maisha yao ("wasiovuta"),[1] adenocarcinoma ni aina ya saratani ya mapafu inayopatikana.[45] Aina ndogo ya adenocarcinoma, bronchioloalveolar carcinoma, hupatikana sana kwa wanawake wasiovuta, na inaweza kuwa na muda nzuri wa kuishi.[46]
Kasinoma ya seli ya squamous huchangia kwa takribani asilimia 30 ya saratani za mapafu. Hutokea kwa njia za hewa zilizokubwa. Kaviti tupu na inayohusishwa kufa kwa seli kwa kawaida hupatikana katikati ya tyuma.[8] Takribani asilimia 9 ya saratani za mapafu ni kasinoma ya seli kubwa. Huitwa hivyo kwa kuwa seli za saratani ni kubwa, na zina cytoplasm nyingi zaidi, nukliasi iliyo kubwa na inayoonekana nucleoli.[8]
Kasinoma ya mapafu ya seli ndogo
[hariri | hariri chanzo]Kasinoma ya mapafu ya seli ndogo (uchunguzi wa sindano ya biopsi kwa kutumia darubini)
Katika kasinoma ya mapafu ya seli ndogo (KMSD), seli huwa na granuli nene zinazotoa neurosisi (vesicles zilizo na homoni), za mfumo wa neva na endokrini zinazopatia tyuma muungano wa sindromu ya endokrini/paraneoplasti.[47] Mara nyingi hutokea katika njia za hewa zilizokubwa zaidi bronkia(za kwanza na za pili).[10] Saratani hizi hukua haraka na kuenea mapema wakati wa maradhi. Asilimia sitini hadi sabini huwa na maradhi ya metastiki inapotokea. Aina hii ya saratani ya mapafu huhusishwa sana na uvutaji.[1]
Zingine
[hariri | hariri chanzo]Aina nyingine nne kuu za histolojia zimetambuliwa, hata ingawa saratani zingine zinaweza kuwa na mchanganyiko wa aina tofauti za aina ndogo.[44] Aina ndogo zilizo nadra hujumuisha tyuma za glandi, tyuma za kasinoidi, na kasinoma zisizopambanuliwa.[1]
Metastasisi
[hariri | hariri chanzo]| Histological type | Immunostain |
|---|---|
| Squamous-cell carcinoma | CK5/6 positive CK7 negative |
| Adenocarcinoma | CK7 positive TTF-1 positive |
| Large-cell carcinoma | TTF-1 negative |
| Small-cell carcinoma | TTF-1 positive CD56 positive Chromogranin positive Synaptophysin positive |
Mapafu ni sehemu ya kawaida ya uenezi wa tyuma kutoka sehemu zingine za mwili. Saratani za pili zimeainishwa kutokana na chanzo chake; kwa mfano, saratani ya matiti iliyoenea kwa mapafu huitwa saratani ya matiti ya metastasisi. Metastasisi mara nyingi huwa na sifa ya kuonekana mviringo kwa radiografu ya kifua.[48]
Saratani za kwanza za mapafu kwa kawaida huenea kwa ubongo, mifupa, ini, na glandi ya adrenali.[8] Immunostaining ya biopsi mara nyingi husaidia kubaini kiini halisi.[49]
Hatua ya saratani
[hariri | hariri chanzo]Hatua ya saratani ni kutathmini maenezi ya saratani kutoka chanzo chake. Ni mojawapo ya masuala yanayoathiri prognosisi na uwezekano wa kutibu saratani ya mapafu.[1]
Utathmini wa kwanza wa hatua ya saratani ya mapafu ya seli kubwa (SMSK) hutumia uainishaji wa TNM. Hii huzingatia ukubwa wa tyuma, limfu huhusishaji nodi na kwa umbalimetastasisi. Baadaye, kwa kutumia kielezi TNM, Kikundi hupeanwa, kuanzia saratani ya kwanza kupitia awamu 0, 1-A (moja A), IB, IIA, IIB, IIIA, IIIB na IV (nne). Kikundi hiki cha awamu husaidia kwa uchaguzi wa matibabu na makadirio ya prognosisi.[50] Kasinoma ya mapafu ya seli ndogo (KMSN) kimapokeo imeainishwa kuwa 'awamu iliyo na mpaka' (iliyofungiwa kwa moja na nusu ya kifua na kati ya eneo la radiotherapi moja inayoweza kustahimiliwa) au 'awamu pana' (magonjwa yaliyoenea pakubwa zaidi).[1] Hata hivyo, uainishaji wa TNM na upangaji ni muhimu kwa kukadiria prognosisi.[50]
Kwa KMSK na KMSK, aina zote mbili za kawaida za utathmini wa hatua ni ule wa kliniki na upasuaji. Hatua ya saratani hubainishwa kabla ya upasuaji wenyewe. Huzingatia matokeo ya masomo ya picha (kama vile uchunguzi wa CT na uchunguzi wa PET) na matokeo ya biopsi. Hatua ya upasuaji hutathminiwa wakati wa au baada ya upasuaji, na huzingatia muunganisho wa matokeo ya upasuaji na kliniki, pamoja na kuchukua sampuli za nodi za limfu za kifua.[8]
UKingaji
[hariri | hariri chanzo]Ukingaji ndio gharama ya chini ya kuzuia kukua kwa saratani ya mapafu. Ilhali katika mataifa mengi kasinojeni za viwanda na zile za nyumbani zimetambuliwa na kupigwa marufuku, uvutaji tumbaku ungali umeenea pakubwa. Kukomesha uvutaji wa tumbaku ni lengo la kwanza katika ukingaji kukomesha uvutaji ni kifaa muhimu katika utaratibu huu.[51]
Sera za kupunguza uvutaji wa moshi ya sigara Kwenye maeneo kama vile hoteli na pahali pa kufanyia kazi umekuwa wa kawaida katika mataifa mengi ya magharibi.[52] Bhutan imepiga marufuku uvutaji wa sigara tangu mwaka wa 2005[53] ilhali India ilipiga marufuku uvutaji wa tumbaku mwezi wa kumi 2008.[54] Shirika la Afya la Ulimwengu limetoa wito kwa serikali kuanzisha upigaji marufuku wa kutangaza tumbaku ili vijana wasianze kuvuta. Hutathmini unaonyesha kuwa uvutaji umepungua kwa asilimia 16%.[55]
Utumiaji wa nyongeza ya vitamini A kwa muda mrefu,[56][57] vitamini C,[56] vitamini D[58] au vitamin E[56] Hupunguzi hatari ya saratani ya mapafu. Uchunguzi mwingine unapendekeza kuwa watu wanaokula chakula kilicho na kiwango cha juu zaidi cha mboga na matunda wana hatari ya chini,[20][59] lakini hii inawezekana kwa sababu ya kushangaza. Uchunguzi mkali zaidi haujaonyesha ushirikiano dhahiri.[59]
Uchunguzi
[hariri | hariri chanzo]Uchunguzi ni matumizi ya uchunguzi wa matibabu ili kubaini ugonjwa kwa watu wanaoonyesha dalili. Uwezekano wa vipimo vya kuchuja saratani ya mapafu ni pamoja na sputum saitolojia, radiografu ya kifua, na tomografia ya digitali. Utaratibu wa uchunguzi unaotumia radiografu ya kifua au saitologia haijaleta manufaa.[60] Kuchuja walio katika hatari kuu (yaani, miaka 55 hadi 79 waliovuta zaidi ya pakiti 30 kwa mwaka au wale wamewahi kupata saratani ya mapafu hapo awali) kwa mwaka na dozi iliyo chini ya uchunguzi wa picha inaweza kupunguza uwezekano wa kifo kutokana na saratani ya mapafu kwa kiasi kamili ya asilimia 0.3 (hatari kiasi ya asilimia 20).[61][62] Hata hivyo, kuna kiwango cha juu ya matokeo duni kinachoweza kusababisha utaratibu wa upasuaji vile vile gharama kubwa ya fedha.[63] Kwa kila tokeo la kipimo halisi kuna zaidi ya 19 ya matokeo duni.[64] Kuwa wazi kwa mnururisho ni njia nyingine ya madhara inayoweza kuwa kutokana na kuchuja.[65]
Udhibiti
[hariri | hariri chanzo]Matibabu ya saratani ya mapafu hulingana na seli maalum ya saratani kuenea, na hali ya utendaji wa mtu. Matibabu ya kawaida hujumuisha huduma ya kupunguza maumivu,[66] upasuaji, kemotherapi, na therapi ya mnururisho.[1]
Upasuaji
[hariri | hariri chanzo]numonektomi sampuli iliyo na squamous-cell carcinoma, inayoonekana nyeupe karibu na bronkia
Ikiwa uchunguzi utathibitisha KSMK, hatua inatathminiwa ili kuamua ikiwa kuna ugonjwa katika eneo maalum na inaweza kutibiwa kwa upasuaji au iwapo imeenea kwa kiwango kisichoweza kufanyiwa upasuaji. Uchunguzi wa picha na picha ya kompyuta ya miale ya gama inatumika kwa uamuzi.[1] Ikiwa unashuku tezi ya mediastinamu inahusika, upasuaji wa mediastinamu inaweza kutumika kutengeneza sampuli nodi na kutathmini kiwango.[67] Upimaji wa damu na uchunguzi wa utendakazi wa mapafu hutumika kutathmini iwapo mtu atafanyiwa upasuaji.[10] Ikiwa matokeo ya uchunguzi wa utendakazi wa mapafu yataonyesha kuwa mapafu hayana hewa ya kutosha, upasuaji hautawezekana.[1]
Katika hali nyingi za kwanza KSMK, kutoa tundu la pafu matibabu ya upasuaji ya (lobektomia) huchaguliwa. Watu wasio sawa kwa lobektomia mzima, sublobar kiasi (kuondoa kipande cha tishu) inaweza kutekelezwa. Hata hivyo, kuondoa kipande hiki kina hatari kubwa ya kurudi tena kuliko lobektomia.[68] Mnururisho iodini brachytherapy ukingoni mwa kuondoa kipande cha tishu unaweza kupunguza hatari ya kurudi tena.[69] Ni nadra, kutoa pafu lote (numonektomi) hufanywa.[68] Upasuaji wa thoracoscopic unaosaidiwa na video na lobektomia ya VATS hutumia njia itakayoingia ndani katika upasuaji.[70] Lobektomia ya VATS inapendekezwa kwa usawa kulingana na lobektomia ya wazi iliyo kawaida, na magonjwa baada ya upasuaji. [71]
Kwa KSMN, kemotherapi na/au radiotherapi hutumika.[72] Hata hivyo jukumu la upasuaji kwa KSMN inastahili kufikiriwa tena. Upasuaji unaweza kuboresha matokeo itakapowekwa kwa kemotherapi na mnururisho katika hatua ya kwanza ya KSMN.[73]
Radiotherapi
[hariri | hariri chanzo]Radiotherapi hutolewa mara kwa mara pamoja na kemotherapi, na inaweza kutumika pamoja na dhamira ya kuponya kwa watu walio na KSMK wasioweza kufanyiwa upasuaji. Hali iliyo kali sana huitwa radiotherapi ya radikali.[74] Mabadiliko ya utaratibu huu hugawanywa kulingana na makali ya radiotherapi unaoendelea, ambapo dozi kali ya radiotherapi hutolewa kwa muda mfupi. [75] Radiotherapi ya kifua baada ya upasuaji haipaswi kutumika baada ya upasuaji wa dhamira ya kuponya kwa watu waliona KSMK.[76] Baadhi ya watu walio na mediastinamu ya limfu nodi ya N2 inayohusika wanaweza kufaidika kutokana na radiotherapi ya baada ya upasuaji.[77]
Kwa hali ya KSMN, radiotherapi mara nyingi inapendekezwa zaidi pamoja na kemotherapi.[8]
Ikiwa ueneaji wa saratani itaziba sehemu ya bronkasi, brachytherapy (radiotherapi maalum) inaweza kupewa moja kwa moja ndani ya njia ya hewa ili njia ifunguke.[78] Kulingana na mwali wa mwanga ya nje ya radiotherapi, brachytherapy inaruhusu kupungua kwa muda wa matibabu na upungufu wa uwazi kwa mnururisho kwa wahudumu wa afya.
Prophylactic cranial irradiation (PCI) ni aina ya radiotherapi kwa akili, hutumika kupunguza hatari ya metastasisi. (PCI) hutumika sana kwa KSMN. Katika hatua za ugonjwa mdogo, (PCI) huongeza miaka mitatu za maisha kutoka asilimia 15 hadi 20; kwa ugonjwa uliozidi, kuishi mwaka mmoja huzidi kutoka asilimia 13 hadi 27.[79]
Maendeleo ya hivi karibuni yanayolenga na kutoa picha yameleta maendeleo ya upasuaji kwa kutumia mnururisho kwa kutibu saratani iliyo katika hatua ya kwanza. Katika aina hii, dozi kali hutolewa kwa idadi ndogo ya vipindi kwa kutumia mbinu ya kulenga upasuaji. Matumizi yake hasa ni kwa wagonjwa wasiofanyiwa upasuaji kwa sababu ya matibabu comorbidities.[80]
Kwa wagonjwa walio na KSMK na KSMN, dozi kiasi cha mnururisho kwa kifua inaweza kutumika ili kudhibiti dalili (radiotherapi ya inayopunguza maumivu).[81]
Kemotherapi
[hariri | hariri chanzo]Mazoezi ya kemotherapi inalingana na aina ya tyuma.[8] Kasinoma ya mapafu ya seli ndogo (KMSN), hata kiasi kidogo ya hatua ya kwanza ya ugonjwa, hutibiwa hasa kwa kemotherapi na mnururisho.[82] Kwa KMSN, cisplatin na etoposide kwa kawaida hutumika zaidi.[83] Zikiunganishwa na carboplatin, gemcitabine, paclitaxel, vinorelbine, topotecan, na irinotecan pia zinatumika.[84][85] Kwa kasinoma ya mapafu ya seli kubwa (KMSK) iliyozidi, kemotherapi huboresha maisha na hutumika kama tiba ya kwanza, bora mtu awe sawa kwa kupokea matibabu.[86] Kwa kawaida, dawa mbili hutumika, moja yazo mara nyingi huwa besi ya platinamu (ama cisplatin au carboplatin). Dawa zingine zinazotumika ni gemcitabine, paclitaxel, docetaxel,[87][88] pemetrexed,[89] etoposide au vinorelbine.[88]
Kemotherapi ya adjuvant inamaanisha matumizi ya kemotherapi baada ya matibabu ya upasuaji ili kuboresha matokeo. Katika KMSK, sampuli huchuliwa karibu na limfu nodi wakati wa upasuaji ili kusaidia hatua. Ikiwa ugonjwa wa kiwango cha II au cha III kitatambulika, kemotherapi ya adjuvanti inaboresha maisha kwa asilimia 5 kwa miaka mitano.[90][91] Matumizi ya vinorelbine pamoja na cisplatin yana matokeo bora kuliko mazoezi.[91] Kemotherapi ya adjuvanti kwa watu waliokuwa na saratani iliyo kiwango IB haijakubalika, kama vipimo vya kliniki havijaonyesha manufaa.[92][93] Vipimo vya kemotherapi kabla ya upasuaji (kemotherapi ya neoadjuvant) kwa KMSK yanayoweza kugawanywa hayajahitimishwa.[94]
Huduma ya kupunguza maumivu
[hariri | hariri chanzo]Kwa wagonjwa walio na ugonjwa usiotibika, huduma ya kupunguza au udhibiti wa hospitali inafaa.[10] Mbinu hizi hukubali majadiliano zaidi ya matibabu na kutoa nafasi kuafikia kwa maamuzi yaliyozingatiwa vilivyo[95][96] na yanaweza kuepushwa na huduma isiyosaidia katika maisha.[96]
Kemotherapi inaweza kuunganishwa na huduma ya kupunguza maumivu kwa matibabu ya KMSK. Kwa hali zilizozidi, kemotherapi inayofaa huboresha maisha wastani zaidi ya huduma ya kusaidia pekee, vile vile kuboresha ubora wa maisha.[97] Pamoja na ubora wa mwili unaofaa, kuendeleza kemotherapi wakati wa kutuliza saratani ya mapafu huzidisha maisha kwa miezi 1.5 hadi 3, kutuliza dalili, na kuboresha maisha, pamoja na matokeo mema zinazoonekana na maajenti wa kisasa.[98][99] Kikundi cha chambuzi cha KMSK inapendekeza kwamba iwapo mgonjwa anahitaji na anaweza kuvumilia matibabu, basi kemotherapi inapaswa kutumiwa kwa KMSK iliyoendelea.[86][100]
Prognosisi
[hariri | hariri chanzo]| Clinical stage | Five-year survival (%) | |
|---|---|---|
| Non-small cell lung carcinoma | Small cell lung carcinoma | |
| IA | 50 | 38 |
| IB | 47 | 21 |
| IIA | 36 | 38 |
| IIB | 26 | 18 |
| IIIA | 19 | 13 |
| IIIB | 7 | 9 |
| IV | 2 | 1 |
Prognosisi huwa duni. Kwa watu wote walio na saratani ya mapafu, asilimia 15 huishi kwa miaka mitano baada ya kutambuliwa.[2] Mara kwa mara kiwango huzidi wakati wa utambuzi. Wakati wa kujitokeza, asilimia 30-40 ya hali ya KMSK huwa kiwango cha IV, na asilimia 60 ya KMSN huwa kiwango cha IV.[8]
Visababishi vya prognosisi katika KMSK ni pamoja na kuwepo na kutokuwepo kwa dalili za mapafu, ukubwa wa tyuma, (histologia) ya aina ya seli, kiwango cha kuenea (hatua) na metastasisi kwa limfu nodi yaliyozidi, na kuathiriwa kwa mishipa. Kwa watu walio na ugonjwa usiofanyiwa upasuaji, matokeo huwa mabaya kwa walio na hali ya utendakazi mbaya na upungufu wa uzito zaidi ya asilimia 10.[101] Visababishi vya prognosisi kwa saratani ya mapafu kwa seli ndogo inahusisha hali ya utendakazi, jinsia, kiwango cha ugonjwa, na kuhusika kwa mfumo wa kati wa neva au ini wakati wa utambuzi.[102]
Kwa KMSK, prognosisi bora imefanikishwa na upasuaji kamili wa kiwango cha IA cha ugonjwa, ikiwa na asilimia 70 ya kuishi miaka mitano.[103] Kwa KMSK, maisha kwa ujumla ni angalau asilimia 5.[1] Watu walio na kiwango kilichozidi cha KMSK kawaida huwa kiasi cha miaka mitano ya kiwango cha maisha iliyo chini ya asilimia 1. Muda wa kawaida wa kuishi wa kiwango kidogo cha ugonjwa ni miezi 20, na kiwango cha miaka mitano za kuishi zilizo asilimia 20.[2]
Kulingana na utafiti wa Taasisi ya kimataifa ya saratani, umri wa kati ya kutambua saratani ya mapafu kule Marekani ni miaka 70,[104] na umri kati ya kifo ni miaka 72.[105] Nchini Marekani, walio na bima ya matibabu hupata matokeo bora zaidi.[106]
Epidemiolojia
[hariri | hariri chanzo]
no data ≤ 5 5-10 10-15 15-20 20-25 25-30 | 30-35 35-40 40-45 45-50 50-55 ≥ 55 |

Ulimwenguni, saratani ya mapafu ni ya kawaida katika swala la tukio na kifo. Katika 2008, kulikuwa na milioni 1.61 za hali mpya, na vifo milioni 1.38 kwa sababu ya saratani ya mapafu. Viwango vilivyo juu sana kiko Uingerezani na Kaskazini Marekani.[11] Sehemu ya watu wanaoweza kupata saratani ya mapafu zaidi ni wale waliozidi umri wa miaka 50 wanao historia ya uvutaji wa sigara. Kwa kutofautisha kiwango cha vifo kwa wanaume, iliyoanza kushuka zaidi miaka ishirini iliyopita, viwango vya vifo kutokana na saratani ya mapafu kwa wanawake vimeongezeka zaidi katika kipindi cha miaka kumi zilizopita, na vinaanza kutulia.[108] Nchini Marekani, hatari ya kupata saratani ya mapafu ni asilimia 8 kwa wanaume na asilimia 6 kwa wanawake. [1]
Kwa kila milioni 3-4 ya sigara iliyovutwa, kifo kimoja hutokea kutokana na saratani ya mapafu.[1][109] Ushawishi wa "Tumbaku Kubwa" huchukua jukumu kubwa katika utamaduni wa uvutaji wa sigara.[110] Vijana wasiovuta sigara wanao tazama matangazo ya uvutaji wa sigara huenda wakavuta.[111] Jukumu la kuvuta moshi ya sigara inaendelea kutambulika kama hatari ya saratani ya mapafu,[24] inayoelekeza kwa sera ya kuingilia upungufu wa wasiovuta kutotaka kuwa karibu wavutaji wanapovuta.[112] Moshi kutoka magari, viwanda, na vituo vya umeme pia vinaweza kuwa hatari.[4]
Ulaya Mashariki ina vifo vilivyosababishwa na saratani ya mapafu vilivyo juu kwa wananume, bali kaskazini mwa Uingereza na Marekani huwa na vifo vingi kwa wanawake. Nchini Marekani, wanaume na wanawake weusi huwa na hali iliyo juu zaidi.[113] Viwango vya saratani kwa sasa viko chini kwa nchi zinazoendelea.[114] Pamoja na ongezeko la uvutaji kwa nchi zinazoendelea, viwango vinatarajiwa kuongezeka kwa miaka michache yanayokuja, hasa Uchina[115] na India.[116]
Kutoka 1960, viwango vya adenocarcinoma vilianza kuzidi kulingana na aina zingine za saratani ya mapafu. Hii ndio sababu ndogo ya kuanzishwa kwa sigara yenye chujio. Matumizi ya chujio hutoa moshi nzito kutoka tumbaku, hivyo kupunguza mabaki kwa njia za kupumua. Hata hivyo, mvutaji lazima avute moshi ndani sana ili apate kiasi sawa cha nikotini, na kuzidisha moshi kuingia kwa njia ndogo za hewa ambapo adenocarcinoma ina panda.[117] Hali ya adenocarcinoma ya mapafu huzidi kupanda.[118]
Historia
[hariri | hariri chanzo]Saratani ya mapafu haikujulikana kabla ya matangazo ya uvutaji wa sigara; haikutambulika kama ugonjwa tofauti hadi mwaka wa 1761.[119] Vipengele tofauti vya saratani ya mapafu yameelezwa zaidi mwaka wa 1810.[120] Tyuma ya mapafu ya kuhatarisha yamechangia asilimia 1 pekee kwa saratani yaliyoonekana kwa otopsi mwaka 1878, lakini yalizidi asilimia 10-15 mwanzoni mwa mwaka 1900.[121] Ripoti za uchunguzi katika maandiko ya matibabu yalikuwa 374 pekee duniani mwaka 1912,[122] lakini uchunguzi wa otopsi ulionyesha hali ya saratani ya mapafu yaliongezeka kutoka asilimia 0.3 mwaka 1852 hadi asilimia 5.66 mwaka 1952.[123] Nchini Ujerumani mwaka 1929, fizishiani Fritz Lickint alitambua uhusiano baina ya uvutaji wa sigara na saratani ya mapafu,[121] iliyoelekeza kwa kampeni ya kupinga uvutaji wa sigara ulio mkali.[124] Uchunguzi ya madaktari wa Uingereza, uliochapishwa wa 1950, ili kuwa ya kwanza epidemiolojia ili kuwa ushahidi kuu ya kiunganishi baina saratani ya mapafu na uvutaji wa sigara.[125] Kama matokeo, mwaka 1964 Mpasuaji Mkuu nchini Marekani aliwashauri wavutaji sigara kuwacha kuvuta.[126]
Uhusiano na gesi ya radoni ulitambuliwa na wachimbuaji wa madini katika Milima za Ore karibu na Schneeberg, Saxony. Fedha ime chimbuliwa hapo tangu mwaka wa 1470, na machimbo haya yana urani nyingi, ikitanguliwa na radiamu na gesi ya radoni.[127] Wachimbuaji madini walipata kiasi isiyolingana na saratani ya mapafu, baadae kujulikana kama saratani ya mapafu mwaka wa 1870.[128] Licha ya utambulizi huu, kuchimbuliwa kulizidi hadi mwaka wa 1950, kwa sababu ya madai ya urani kutoka Urusi.[127] Radoni ilitambulika kama kisababishi cha saratani ya mapafu mwaka wa 1960.[129]
Mafanikio ya kwanza ya numonektomi ya saratani ya mapafu ulifanywa mwaka wa 1933.[130] Radiotherapi ya kupunguza maumivu imetumika tangu mwaka wa 1940.[131] Radiotherapi ya radikali, iliyotumika awali mwaka wa 1950, ilikuwa jaribio la kutumia dozi kubwa ya mnururisho kwa wagonjwa walio na kiasi cha saratani kinachoanza, lakini hawawezi kufanyiwa upasuaji vinginevyo.[132] Mwaka wa 1997, mkeneko mkali wa radiotherapi uliochapuzwa unaoendelea ulionekana ukiendelea kuliko radiotherapi ya radikali iliyo ya kawaida.[133] Kwa SMSD, majaribio ya hapo awali mwaka wa 1960 katika upasuaji [134] na radiotherapi ya radikali[135] hayakufaulu. Mwaka wa 1970, kemotherapi ya mazoezi yaliyofaulu yaliendelezwa.[136]
Marejeo
[hariri | hariri chanzo]- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 Horn, L (2012). "Chapter 89". Katika Longo, DL; Kasper, DL; Jameson, JL; Fauci, AS; Hauser, SL; Loscalzo, J (whr.). Harrison's Principles of Internal Medicine (tol. la 18th). McGraw-Hill. ISBN 0-07-174889-X.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ↑ 2.0 2.1 2.2 2.3 "Lung Carcinoma: Tumors of the Lungs". Merck Manual Professional Edition, Online edition. Iliwekwa mnamo 2007-08-15.
- ↑ Thun, MJ (2008). "Lung cancer occurrence in never-smokers: an analysis of 13 cohorts and 22 cancer registry studies". PLoS Medicine. 5 (9): e185. doi:10.1371/journal.pmed.0050185. PMC 2531137. PMID 18788891.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help)CS1 maint: unflagged free DOI (link) - ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 Alberg AJ, Samet JM (2010). "Chapter 46". Murray & Nadel's Textbook of Respiratory Medicine (tol. la 5th). Saunders Elsevier. ISBN 978-1-4160-4710-0.
- ↑ 5.0 5.1 O'Reilly, KM (2007). "Asbestos-related lung disease". American Family Physician. 75 (5): 683–688. PMID 17375514. Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo 2007-09-29. Iliwekwa mnamo 2014-01-09.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|dead-url=ignored (|url-status=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Carmona, RH (2006-06-27). "The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General". U.S. Department of Health and Human Services.
Secondhand smoke exposure causes disease and premature death in children and adults who do not smoke.
- ↑ "Tobacco Smoke and Involuntary Smoking" (PDF). IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. 83. WHO International Agency for Research on Cancer. 2002.
There is sufficient evidence that involuntary smoking (exposure to secondhand or 'environmental' tobacco smoke) causes lung cancer in humans. ... Involuntary smoking (exposure to secondhand or 'environmental' tobacco smoke) is carcinogenic to humans (Group 1).
- ↑ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 Lu, C (2010). "78: Cancer of the Lung". Holland-Frei Cancer Medicine (tol. la 8th). People's Medical Publishing House. ISBN 9781607950141.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ↑ Chapman, S (2009). "Chapter 31". Oxford Handbook of Respiratory Medicine (tol. la 2nd). Oxford University Press. ISBN 9-780199-545162.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ↑ 10.0 10.1 10.2 10.3 10.4 10.5 Collins, LG (2007). "Lung cancer: diagnosis and management". American Family Physician. 75 (1). American Academy of Family Physicians: 56–63. PMID 17225705. Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo 2007-09-29. Iliwekwa mnamo 2014-01-09.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|dead-url=ignored (|url-status=suggested) (help); Unknown parameter|month=ignored (help) - ↑ 11.0 11.1 Ferlay, J (Desemba 2010). "Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008". International Journal of Cancer. 127 (12): 2893–2917. doi:10.1002/ijc.25516. PMID 21351269.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: date auto-translated (link) - ↑ Honnorat, J (2007). "Paraneoplastic neurological syndromes". Orphanet Journal of Rare Diseases. 2 (1). BioMed Central: 22. doi:10.1186/1750-1172-2-22. PMC 1868710. PMID 17480225.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help)CS1 maint: unflagged free DOI (link) - ↑ Greene, Frederick L. (2002). AJCC cancer staging manual. Berlin: Springer-Verlag. ISBN 0-387-95271-3.
- ↑ Brown, KM (2010). "8". Holland-Frei Cancer Medicine (tol. la 8th). People's Medical Publishing House USA. ISBN 978-1607950141.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ↑ Biesalski, HK (1998). "European Consensus Statement on Lung Cancer: risk factors and prevention. Lung Cancer Panel". CA Cancer J Clin. 48 (3). Smoking is the major risk factor, accounting for about 90% of lung cancer incidence.: 167–176, discussion 164–166. doi:10.3322/canjclin.48.3.167. PMID 9594919.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: location (link) - ↑ Hecht, S (2003). "Tobacco carcinogens, their biomarkers and tobacco-induced cancer". Nature Reviews Cancer. 3 (10). Nature Publishing Group: 733–744. doi:10.1038/nrc1190. PMID 14570033.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Sopori, M (2002). "Effects of cigarette smoke on the immune system". Nature Reviews Immunology. 2 (5): 372–7. doi:10.1038/nri803. PMID 12033743.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Peto, R (2006). Mortality from smoking in developed countries 1950–2000: Indirect estimates from National Vital Statistics. Oxford University Press. ISBN 0-19-262535-7.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ↑ California Environmental Protection Agency (1997). "Health effects of exposure to environmental tobacco smokeCalifornia Environmental Protection Agency". Tobacco Control. 6 (4): 346–353. doi:10.1136/tc.6.4.346. PMC 1759599. PMID 9583639.
* CDC (2001). "State-specific prevalence of current cigarette smoking among adults, and policies and attitudes about secondhand smoke—United States, 2000". Morbidity and Mortality Weekly Report. 50 (49). Atlanta, Georgia: CDC: 1101–1106. PMID 11794619.{{cite journal}}: More than one of|author1=na|last=specified (help); Unknown parameter|month=ignored (help) - ↑ 20.0 20.1 20.2 20.3 Alberg, AJ (2007). "Epidemiology of lung cancer". Chest. 132 (S3). American College of Chest Physicians: 29S–55S. doi:10.1378/chest.07-1347. PMID 17873159. Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo 2020-03-29. Iliwekwa mnamo 2014-01-09.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|dead-url=ignored (|url-status=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Jaakkola, MS (2006). "Impact of smoke-free workplace legislation on exposures and health: possibilities for prevention". European Respiratory Journal. 28 (2): 397–408. doi:10.1183/09031936.06.00001306. PMID 16880370.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Parkin, DM (2011). "Tobacco—attributable cancer burden in the UK in 2010". British Journal of Cancer. 105 (Suppl. 2): S6–S13. doi:10.1038/bjc.2011.475. PMC 3252064. PMID 22158323.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ National Health and Medical Research Council (Aprili 1994). "The health effects and regulation of passive smoking". Australian Government Publishing Service. Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo Septemba 29, 2007. Iliwekwa mnamo 2007-08-10.
{{cite journal}}: Cite journal requires|journal=(help)CS1 maint: date auto-translated (link) - ↑ 24.0 24.1 Taylor, R (2007). "Meta-analysis of studies of passive smoking and lung cancer: effects of study type and continent". International Journal of Epidemiology. 36 (5): 1048–1059. doi:10.1093/ije/dym158. PMID 17690135.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ "Frequently asked questions about second hand smoke". World Health Organization. Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo 2013-01-01. Iliwekwa mnamo 25 Julai 2012.
{{cite web}}: CS1 maint: date auto-translated (link) - ↑ Schick, S (2005). "Philip Morris toxicological experiments with fresh sidestream smoke: more toxic than mainstream smoke". Tobacco Control. 14 (6): 396–404. doi:10.1136/tc.2005.011288. PMC 1748121. PMID 16319363.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Schmid K, Kuwert T, Drexler H (2010). "Radon in Indoor Spaces: An Underestimated Risk Factor for Lung Cancer in Environmental Medicine". Dtsch Arztebl Int. 107 (11): 181–6. doi:10.3238/arztebl.2010.0181. PMC 2853156. PMID 20386676.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ EPA (2006). "Radiation information: radon". EPA. Iliwekwa mnamo 2007-08-11.
{{cite web}}: Unknown parameter|month=ignored (help) - ↑ Daviesfirst=RJO (2010). "18.19.3". Oxford Textbook Medicine (tol. la 5th). OUP Oxford. ISBN 978-0199204854.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ↑ Chen, H (2008). "A systematic review of the relation between long-term exposure to ambient air pollution and chronic diseases". Reviews on Environmental Health. 23 (4): 243–297. PMID 19235364.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Clapp, RW (2008). "Environmental and Occupational Causes of Cancer New Evidence, 2005–2007". Reviews on Environmental Health. 23 (1): 1–37. PMC 2791455. PMID 18557596.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ 32.0 32.1 Lim, WY (2012 Jan). "Biomass fuels and lung cancer". Respirology (Carlton, Vic.). 17 (1): 20–31. PMID 22008241.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ↑ 33.0 33.1 Sood, A (2012 Dec). "Indoor fuel exposure and the lung in both developing and developed countries: an update". Clinics in chest medicine. 33 (4): 649–65. PMID 23153607.
{{cite journal}}: Check date values in:|date=(help) - ↑ Dudley, Joel (2013). Exploring Personal Genomics. Oxford University Press. uk. 25. ISBN 9780199644483.
- ↑ Kern JA, McLennan G (2008). Fishman's Pulmonary Diseases and Disorders (tol. la 4th). McGraw-Hill. uk. 1802. ISBN 0-07-145739-9.
- ↑ Cogliano, VJ (2011 Dec 21). "Preventable exposures associated with human cancers" (PDF). Journal of the National Cancer Institute. 103 (24): 1827–39. PMID 22158127. Ilihifadhiwa kwenye nyaraka kutoka chanzo (PDF) mnamo 2012-09-20. Iliwekwa mnamo 2014-01-09.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|dead-url=ignored (|url-status=suggested) (help) - ↑ Fong, KM (2003). "Lung cancer • 9: Molecular biology of lung cancer: clinical implications". Thorax. 58 (10). BMJ Publishing Group Ltd.: 892–900. doi:10.1136/thorax.58.10.892. PMC 1746489. PMID 14514947.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Salgia, R (1998). "Molecular abnormalities in lung cancer". Journal of Clinical Oncology. 16 (3): 1207–1217. PMID 9508209.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ 39.0 39.1 39.2 39.3 Herbst, RS (2008). "Lung cancer". New England Journal of Medicine. 359 (13): 1367–1380. doi:10.1056/NEJMra0802714. PMID 18815398. Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo 2008-09-28. Iliwekwa mnamo 2014-01-09.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|dead-url=ignored (|url-status=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Aviel-Ronen, S (2006). "K-ras mutations in non-small-cell lung carcinoma: a review". Clinical Lung Cancer. 8 (1). Cancer Information Group: 30–38. doi:10.3816/CLC.2006.n.030. PMID 16870043.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Devereux, TR (1996). "Molecular mechanisms of lung cancer. Interaction of environmental and genetic factors". Chest. 109 (Suppl 3). American College of Chest Physicians: 14S–19S. doi:10.1378/chest.109.3_Supplement.14S. PMID 8598134.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Miller, WT (2008). Fishman's Pulmonary Diseases and Disorders (tol. la 4th). McGraw-Hill. uk. 486. ISBN 0-07-145739-9.
- ↑ Kaiser, LR (2008). Fishman's Pulmonary Diseases and Disorders (tol. la 4th). McGraw-Hill. ku. 1815–1816. ISBN 0-07-145739-9.
- ↑ 44.0 44.1 Maitra, A (2007). Robbins Basic Pathology (tol. la 8th). Saunders Elsevier. ku. 528–529. ISBN 978-1-4160-2973-1.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ↑ Subramanian, J (2007). "Lung cancer in never smokers: a review". Journal of Clinical Oncology. 25 (5). American Society of Clinical Oncology: 561–570. doi:10.1200/JCO.2006.06.8015. PMID 17290066.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Raz, DJ (2006). "Bronchioloalveolar carcinoma: a review". Clinical Lung Cancer. 7 (5): 313–322. doi:10.3816/CLC.2006.n.012. PMID 16640802.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Rosti, G (2006). "Small cell lung cancer". Annals of Oncology. 17 (Suppl. 2): 5–10. doi:10.1093/annonc/mdj910. PMID 16608983.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Seo, JB (1 Machi 2001). "Atypical pulmonary metastases: spectrum of radiologic findings". Radiographics. 21 (2): 403–417. PMID 11259704.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: date auto-translated (link) - ↑ Tan D, Zander DS (2008). "Immunohistochemistry for Assessment of Pulmonary and Pleural Neoplasms: A Review and Update". Int J Clin Exp Pathol. 1 (1): 19–31. PMC 2480532. PMID 18784820.
- ↑ 50.0 50.1 50.2 Rami-Porta, R (2009). "The revised TNM staging system for lung cancer" (PDF). Annals of Thoracic and Cardiovascular Surgery. 15 (1): 4–9. PMID 19262443.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Goodman, GE (2002). "Lung cancer. 1: prevention of lung cancer" (PDF). Thorax. 57 (11): 994–999. PMC 1746232. PMID 12403886.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ McNabola, A (2009). "The control of environmental tobacco smoke: a policy review". International Journal of Environmental Research and Public Health. 6 (2): 741–758. doi:10.3390/ijerph6020741. PMC 2672352. PMID 19440413.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help)CS1 maint: unflagged free DOI (link) - ↑ Pandey, G. "Bhutan's smokers face public ban", BBC. Retrieved on 2007-09-07.
- ↑ Pandey, G. "Indian ban on smoking in public", BBC, 2 October 2008. Retrieved on 2012-04-25.
- ↑ UN health agency calls for total ban on tobacco advertising to protect young (Press release). United Nations News service. 30 May 2008. http://www.un.org/apps/news/story.asp?NewsID=26857.
- ↑ 56.0 56.1 56.2 Fabricius, P (2003). "Diet and lung cancer". Monaldi Archives for Chest Disease. 59 (3): 207–211. PMID 15065316.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Fritz, H (2011). "Vitamin A and Retinoid Derivatives for Lung Cancer: A Systematic Review and Meta Analysis". PLoS ONE. 6 (6): e21107. doi:10.1371/journal.pone.0021107. PMC 3124481. PMID 21738614.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: unflagged free DOI (link) - ↑ Herr, C (2011). "The role of vitamin D in pulmonary disease: COPD, asthma, infection, and cancer". Respiratory Research. 12 (1): 31. doi:10.1186/1465-9921-12-31. PMC 3071319. PMID 21418564.
{{cite journal}}: Unknown parameter|month=ignored (help); Unknown parameter|scoauthors=ignored (help)CS1 maint: unflagged free DOI (link) - ↑ 59.0 59.1 Key, TJ (2011). "Fruit and vegetables and cancer risk". British Journal of Cancer. 104 (1): 6–11. doi:10.1038/sj.bjc.6606032. PMC 3039795. PMID 21119663.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Manser, RL (2004). "Screening for lung cancer". Cochrane Database of Systematic Reviews (1): CD001991. doi:10.1002/14651858.CD001991.pub2. PMID 14973979.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ↑ Jaklitsch, MT (2012). "The American Association for Thoracic Surgery guidelines for lung cancer screening using low-dose computed tomography scans for lung cancer survivors and other high-risk groups". Journal of Thoracic and Cardiovascular Surgery. 144 (1): 33–38. doi:10.1016/j.jtcvs.2012.05.060. PMID 22710039.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Bach, PB (2012). "Benefits and harms of CT screening for lung cancer: a systematic review". JAMA: the Journal of the American Medical Association. 307 (22): 2418–2429. doi:10.1001/jama.2012.5521. PMID 22610500.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Boiselle, PM (2013 Mar 20). "Computed tomography screening for lung cancer". JAMA : the journal of the American Medical Association. 309 (11): 1163–70. PMID 23512063.
{{cite journal}}: Check date values in:|date=(help) - ↑ Bach PB, Mirkin JN, Oliver TK; na wenz. (2012). "Benefits and harms of CT screening for lung cancer: a systematic review". JAMA. 307 (22): 2418–29. doi:10.1001/jama.2012.5521. PMID 22610500.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Aberle, DR (2013 Mar 10). "Computed tomography screening for lung cancer: has it finally arrived? Implications of the national lung screening trial". Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 31 (8): 1002–8. PMID 23401434.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ↑ Ferrell, B (2011). "Palliative care in lung cancer". Surgical Clinics of North America. 91 (2): 403–417. doi:10.1016/j.suc.2010.12.003. PMID 21419260.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Kaiser LR (2008). Fishman's Pulmonary Diseases and Disorders (tol. la 4th). McGraw-Hill. ku. 1853–1854. ISBN 0-07-145739-9.
- ↑ 68.0 68.1 Kaiser LR (2008). Fishman's Pulmonary Diseases and Disorders (tol. la 4th). McGraw-Hill. ku. 1855–1856. ISBN 0-07-145739-9.
- ↑ Odell, DD (2010). "Sublobar resection with brachytherapy mesh for stage I non-small cell lung cancer". Seminars in Thoracic and Cardiovascular Surgery. 22 (1): 32–37. doi:10.1053/j.semtcvs.2010.04.003. PMID 20813314.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Alam, N (2007). "Video-assisted thoracic surgery (VATS) lobectomy: the evidence base". Journal of the Society of Laparoendoscopic Surgeons. 11 (3): 368–374. PMC 3015831. PMID 17931521.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Rueth, NM (2010). "Is VATS lobectomy better: perioperatively, biologically and oncologically?". Annals of Thoracic Surgery. 89 (6): S2107–S2111. doi:10.1016/j.athoracsur.2010.03.020. PMID 20493991.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Simon GR, Turrisi A (2007). "Management of small cell lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition)". Chest. 132 (3 Suppl): 324S–339S. doi:10.1378/chest.07-1385. PMID 17873178.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Goldstein, SD (2011). "Role of surgery in small cell lung cancer". Surgical Oncology Clinics of North America. 20 (4): 769–777. doi:10.1016/j.soc.2011.08.001. PMID 21986271.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Arriagada, R (2002). Oxford Textbook of Oncology (tol. la 2nd). Oxford University Press. uk. 2094. ISBN 0-19-262926-3.
{{cite book}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ↑ Hatton, MQ (2010). "Continuous hyperfractionated accelerated radiotherapy (CHART) and non-conventionally fractionated radiotherapy in the treatment of non-small cell lung cancer: a review and consideration of future directions". Clinical Oncology (Royal College of Radiologists). 22 (5): 356–364. doi:10.1016/j.clon.2010.03.010. PMID 20399629.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ PORT Meta-analysis Trialists Group (2005). Rydzewska, Larysa (mhr.). "Postoperative radiotherapy for non-small cell lung cancer". Cochrane Database of Systematic Reviews (2): CD002142. doi:10.1002/14651858.CD002142.pub2. PMID 15846628.
- ↑ Le Péchoux, C (2011). "Role of postoperative radiotherapy in resected non-small cell lung cancer: a reassessment based on new data". Oncologist. 16 (5): 672–681. doi:10.1634/theoncologist.2010-0150. PMC 3228187. PMID 21378080.
- ↑ Cardona, AF (2008). "Palliative endobronchial brachytherapy for non-small cell lung cancer". Cochrane Database of Systematic Reviews (2): CD004284. doi:10.1002/14651858.CD004284.pub2. PMID 18425900.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Paumier, A (2011). "Prophylactic cranial irradiation in lung cancer". Cancer Treatment Reviews. 37 (4): 261–265. doi:10.1016/j.ctrv.2010.08.009. PMID 20934256.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Girard, N (2011). "Stereotactic radiotherapy for non-small cell lung cancer: From concept to clinical reality. 2011 update". Cancer Radiothérapie. 15 (6–7): 522–526. doi:10.1016/j.canrad.2011.07.241. PMID 21889901.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Fairchild, A (2008). "Palliative thoracic radiotherapy for lung cancer: a systematic review". Journal of Clinical Oncology. 26 (24): 4001–4011. doi:10.1200/JCO.2007.15.3312. PMID 18711191.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Hann CL, Rudin CM (2008-11-30). "Management of small-cell lung cancer: incremental changes but hope for the future". Oncology (Williston Park). 22 (13): 1486–92. PMID 19133604.
- ↑ Murray, N (2006). "A review of first-line treatment for small-cell lung cancer". Journal of Thoracic Oncology. 1 (3): 270–278. PMID 17409868.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Azim, HA (2007). "Treatment options for relapsed small-cell lung cancer". Anticancer drugs. 18 (3): 255–261. doi:10.1097/CAD.0b013e328011a547. PMID 17264756.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ MacCallum, C (2006). "Second-line treatment of small-cell lung cancer". Current Oncology Reports. 8 (4): 258–264. doi:10.1007/s11912-006-0030-8. PMID 17254525.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ 86.0 86.1 NSCLC Meta-Analyses Collaborative Group (2008). "Chemotherapy in Addition to Supportive Care Improves Survival in Advanced Non–Small-Cell Lung Cancer: A Systematic Review and Meta-Analysis of Individual Patient Data From 16 Randomized Controlled Trials". J. Clin. Oncol. 26 (28): 4617–25. doi:10.1200/JCO.2008.17.7162. PMC 2653127. PMID 18678835.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Mehra R, Treat J (2008). Fishman's Pulmonary Diseases and Disorders (tol. la 4th). McGraw-Hill. uk. 1876. ISBN 0-07-145739-9.
- ↑ 88.0 88.1 Clegg, A (2002). "Clinical and cost effectiveness of paclitaxel, docetaxel, gemcitabine, and vinorelbine in non-small cell lung cancer: a systematic review". Thorax. 57 (1). BMJ Publishing Group: 20–28. doi:10.1136/thorax.57.1.20. PMC 1746188. PMID 11809985.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Fuld AD, Dragnev KH, Rigas JR (2010). "Pemetrexed in advanced non-small-cell lung cancer". Expert Opin Pharmacother. 11 (8): 1387–402. doi:10.1517/14656566.2010.482560. PMID 20446853.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Carbone, DP (2011). "Adjuvant therapy in non-small cell lung cancer: future treatment prospects and paradigms". Clinical Lung Cancer. 12 (5): 261–271. doi:10.1016/j.cllc.2011.06.002. PMID 21831720.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ 91.0 91.1 Le Chevalier, T (2010). "Adjuvant chemotherapy for resectable non-small-cell lung cancer: where is it going?". Annals of Oncology. 21 (Suppl. 7): vii196–198. doi:10.1093/annonc/mdq376. PMID 20943614.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Horn, L (2007). "The rationale for adjuvant chemotherapy in stage I non-small cell lung cancer". Journal of Thoracic Oncology. 2 (5): 377–383. doi:10.1097/01.JTO.0000268669.64625.bb. PMID 17473651.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Wakelee, HA (2006). "Current status of adjuvant chemotherapy for stage IB non-small-cell lung cancer: implications for the New Intergroup Trial". Clinical Lung Cancer. 8 (1). Cancer Information Group: 18–21. doi:10.3816/CLC.2006.n.028. PMID 16870041.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ BMJ (2005). Clinical evidence concise : the international resource of the best available evidence for effective health care. London: BMJ Publishing Group. ku. 486–488. ISBN 1-905545-00-2. ISSN 1475-9225.
{{cite book}}: Unknown parameter|month=ignored (help) - ↑ Kelley AS, Meier DE (2010). "Palliative care—a shifting paradigm". New England Journal of Medicine. 363 (8): 781–2. doi:10.1056/NEJMe1004139. PMID 20818881.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ 96.0 96.1 Prince-Paul M (2009). "When hospice is the best option: an opportunity to redefine goals". Oncology (Williston Park, N.Y.). 23 (4 Suppl Nurse Ed): 13–7. PMID 19856592.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Souquet PJ, Chauvin F, Boissel JP, Bernard JP (1995). "Meta-analysis of randomised trials of systemic chemotherapy versus supportive treatment in non-resectable non-small cell lung cancer". Lung Cancer. 12 Suppl 1: S147–54. doi:10.1016/0169-5002(95)00430-9. PMID 7551923.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Sörenson S, Glimelius B, Nygren P (2001). "A systematic overview of chemotherapy effects in non-small cell lung cancer". Acta Oncol. 40 (2–3): 327–39. PMID 11441939.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Clegg A, Scott DA, Sidhu M, Hewitson P, Waugh N (2001). "A rapid and systematic review of the clinical effectiveness and cost-effectiveness of paclitaxel, docetaxel, gemcitabine and vinorelbine in non-small-cell lung cancer". Health Technol Assess. 5 (32): 1–195. PMID 12065068.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Kigezo:Cite Cochrane
- ↑ "Non-Small Cell Lung Cancer Treatment". PDQ for Health Professionals. National Cancer Institute. Iliwekwa mnamo 2008-11-22.
- ↑ "Small Cell Lung Cancer Treatment". PDQ for Health Professionals. National Cancer Institute. 2012. Iliwekwa mnamo 2012-05-16.
- ↑ Spiro, SG (2010). "18.19.1". Oxford Textbook Medicine (tol. la 5th). OUP Oxford. ISBN 978-0199204854.
- ↑ SEER data (SEER.cancer.gov)Median Age of Cancer Patients at Diagnosis 2002-2003
- ↑ SEER data (SEER.cancer.gov)Median Age of Cancer Patients at Death 2002-2006
- ↑ Slatore, CG (Novemba 2010). "An official American Thoracic Society systematic review: insurance status and disparities in lung cancer practices and outcomes". American Journal of Respiratory and Critical Care Medicine. 182 (9): 1195–1205. doi:10.1164/rccm.2009-038ST. PMID 21041563.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: date auto-translated (link) - ↑ "WHO Disease and injury country estimates". World Health Organization. 2009. Iliwekwa mnamo Novemba 11, 2009.
{{cite web}}: CS1 maint: date auto-translated (link) - ↑ Jemal A, Tiwari RC, Murray T; na wenz. (2004). "Cancer statistics, 2004". CA: a Cancer Journal for Clinicians. 54 (1): 8–29. doi:10.3322/canjclin.54.1.8. PMID 14974761.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ↑ Proctor, RN (2012). "The history of the discovery of the cigarette-lung cancer link: evidentiary traditions, corporate denial, global toll". Tobacco Control. 21 (2): 87–91. doi:10.1136/tobaccocontrol-2011-050338. PMID 22345227.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Lum, KL (2008). "Signed, sealed and delivered: "big tobacco" in Hollywood, 1927–1951". Tobacco Control. 17 (5): 313–323. doi:10.1136/tc.2008.025445. PMC 2602591. PMID 18818225.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Lovato, C (Oktoba 2011). "Impact of tobacco advertising and promotion on increasing adolescent smoking behaviours". Cochrane Database of Systematic Reviews (10): CD003439. doi:10.1002/14651858.CD003439.pub2. PMID 21975739.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: date auto-translated (link) - ↑ Kemp, FB (2009). "Smoke free policies in Europe. An overview". Pneumologia. 58 (3): 155–158. PMID 19817310.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ National Cancer Institute; SEER stat fact sheets: Lung and Bronchus. Surveillance Epidemiology and End Results. 2010[1]
- ↑ "Gender in lung cancer and smoking research" (PDF). World Health Organization. 2004. Iliwekwa mnamo 2007-05-26.
- ↑ Zhang, J (Novemba 2011). "Tobacco smoking in China: prevalence, disease burden, challenges and future strategies". Respirology. 16 (8): 1165–1172. doi:10.1111/j.1440-1843.2011.02062.x. PMID 21910781.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: date auto-translated (link) - ↑ Behera, D (2004). "Lung cancer in India" (PDF). Indian Journal of Chest Diseases and Allied Sciences. 46 (4): 269–281. PMID 15515828. Ilihifadhiwa kwenye nyaraka kutoka chanzo (PDF) mnamo 2008-12-17. Iliwekwa mnamo 2014-01-09.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|dead-url=ignored (|url-status=suggested) (help) - ↑ Charloux, A (1997). "The increasing incidence of lung adenocarcinoma: reality or artefact? A review of the epidemiology of lung adenocarcinoma". International Journal of Epidemiology. 26 (1): 14–23. doi:10.1093/ije/26.1.14. PMID 9126499.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Kadara, H (2012). "Pulmonary adenocarcinoma: a renewed entity in 2011". Respirology. 17 (1): 50–65. doi:10.1111/j.1440-1843.2011.02095.x. PMID 22040022.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Morgagni, Giovanni Battista (1761). De sedibus et causis morborum per anatomen indagatis. OL 24830495M.
- ↑ Bayle, Gaspard-Laurent (1810). Recherches sur la phthisie pulmonaire (kwa French). Paris. OL 15355651W.
{{cite book}}: CS1 maint: unrecognized language (link) - ↑ 121.0 121.1 Witschi, H (2001). "A short history of lung cancer". Toxicological Sciences. 64 (1): 4–6. doi:10.1093/toxsci/64.1.4. PMID 11606795.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Adler, I (1912). Primary Malignant Growths of the Lungs and Bronchi. New York: Longmans, Green, and Company. OCLC 14783544. OL 24396062M., cited in Spiro SG, Silvestri GA (2005). "One hundred years of lung cancer". American Journal of Respiratory and Critical Care Medicine. 172 (5): 523–529. doi:10.1164/rccm.200504-531OE. PMID 15961694.
- ↑ Grannis, FW. "History of cigarette smoking and lung cancer". smokinglungs.com. Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo 2007-07-18. Iliwekwa mnamo 2007-08-06.
- ↑ Proctor, R (2000). The Nazi War on Cancer. Princeton University Press. ku. 173–246. ISBN 0-691-00196-0.
- ↑ Doll, R (1956). "Lung Cancer and Other Causes of Death in Relation to Smoking". British Medical Journal. 2 (5001): 1071–1081. doi:10.1136/bmj.2.5001.1071. PMC 2035864. PMID 13364389.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ US Department of Health Education and Welfare (1964). "Smoking and health: report of the advisory committee to the Surgeon General of the Public Health Service" (PDF). Washington, DC: US Government Printing Office.
- ↑ 127.0 127.1 Greaves, M (2000). Cancer: the Evolutionary Legacy. Oxford University Press. ku. 196–197. ISBN 0-19-262835-6.
- ↑ Greenberg, M (1993). "Lung cancer in the Schneeberg mines: a reappraisal of the data reported by Harting and Hesse in 1879". Annals of Occupational Hygiene. 37 (1): 5–14. PMID 8460878.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Samet, JM (2011). "Radiation and cancer risk: a continuing challenge for epidemiologists". Environmental Health. 10 (Suppl. 1): S4. doi:10.1186/1476-069X-10-S1-S4. PMC 3073196. PMID 21489214.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: unflagged free DOI (link) - ↑ Horn, L (2008). "Evarts A. Graham and the first pneumonectomy for lung cancer". Journal of Clinical Oncology. 26 (19): 3268–3275. doi:10.1200/JCO.2008.16.8260. PMID 18591561. Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo 2020-03-17. Iliwekwa mnamo 2014-01-09.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|dead-url=ignored (|url-status=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Edwards, AT (1946). "Carcinoma of the Bronchus". Thorax. 1 (1): 1–25. doi:10.1136/thx.1.1.1. PMC 1018207. PMID 20986395.
- ↑ Kabela, M (1956). "Erfahrungen mit der radikalen Röntgenbestrahlung des Bronchienkrebses". Ceskoslovenská Onkológia (kwa German). 3 (2): 109–115. PMID 13383622.
{{cite journal}}: Unknown parameter|trans_title=ignored (|trans-title=suggested) (help)CS1 maint: unrecognized language (link) - ↑ Saunders, M (1997). "Continuous hyperfractionated accelerated radiotherapy (CHART) versus conventional radiotherapy in non-small-cell lung cancer: a randomised multicentre trial". Lancet. 350 (9072). Elsevier: 161–165. doi:10.1016/S0140-6736(97)06305-8. PMID 9250182.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Lennox, SC (1968). "Results of resection for oat-cell carcinoma of the lung". Lancet. 2 (7575). Elsevier: 925–927. doi:10.1016/S0140-6736(68)91163-X. PMID 4176258.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Miller, AB (1969). "Five-year follow-up of the Medical Research Council comparative trial of surgery and radiotherapy for the primary treatment of small-celled or oat-celled carcinoma of the bronchus". Lancet. 2 (7619). Elsevier: 501–505. doi:10.1016/S0140-6736(69)90212-8. PMID 4184834.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help); Unknown parameter|month=ignored (help) - ↑ Cohen, M (1977). "Intensive chemotherapy of small cell bronchogenic carcinoma". Cancer Treatment Reports. 61 (3): 349–354. PMID 194691.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)
- CS1 errors: unsupported parameter
- CS1 maint: unflagged free DOI
- CS1 maint: date auto-translated
- CS1 maint: location
- CS1 errors: redundant parameter
- CS1 errors: missing periodical
- CS1 maint: multiple names: authors list
- CS1 errors: dates
- CS1 errors: explicit use of et al.
- CS1: long volume value
- CS1 maint: unrecognized language
- Kurasa zenye viungo vilivyovunjika
- Saratani
- Mapafu